Free Healthcare Compliance Risk Assessment

Prepared by: [Your Name]
Compliance Officer
Date: January 15, 2050
I. Introduction
The purpose of this Healthcare Compliance Risk Assessment is to identify and mitigate compliance risks associated with healthcare regulations and standards at [Your Company Name], located at [Your Company Address]. This assessment serves as a crucial tool to ensure adherence to various regulatory frameworks, including HIPAA, Medicare, and Medicaid regulations, thereby safeguarding patient data and maintaining the integrity of healthcare operations.
II. Methodology
The assessment employs a comprehensive approach, utilizing both qualitative and quantitative methods to evaluate potential compliance risks. This includes a review of existing policies and procedures, stakeholder interviews, and an analysis of historical compliance issues within the organization.
III. Risk Identification
A thorough identification of potential compliance risks will focus on the following areas:
Regulatory Compliance
Risk Area | Description |
|---|---|
HIPAA Compliance | Risks associated with the unauthorized access to patient records. |
Billing and Coding | Potential errors in coding leading to improper billing practices. |
Operational Compliance
Risk Area | Description |
|---|---|
Staff Training | Inadequate training leading to non-compliance with regulations. |
Vendor Management | Risks arising from third-party vendor compliance issues. |
Data Security
Risk Area | Description |
|---|---|
Cybersecurity Threats | Vulnerabilities to unauthorized data access or breaches. |
Data Loss | Risks associated with potential loss of sensitive information. |
IV. Risk Analysis
Each identified risk will be analyzed based on its likelihood of occurrence and the potential impact on the organization. The following matrix outlines the assessment:
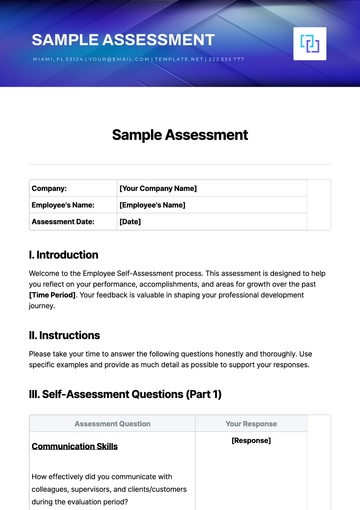
Risk Area | Likelihood (1-5) | Impact (1-5) | Risk Level (Likelihood x Impact) |
|---|---|---|---|
HIPAA Compliance | 3 | 5 | 15 |
Billing and Coding | 4 | 4 | 16 |
Staff Training | 2 | 4 | 8 |
Vendor Management | 3 | 3 | 9 |
Cybersecurity Threats | 4 | 5 | 20 |
Data Loss | 3 | 4 | 12 |
V. Recommendations
Based on the analysis, the following recommendations will be implemented to mitigate identified risks:
Regulatory Compliance
Enhance HIPAA Training: Conduct mandatory training sessions for all staff to ensure understanding and adherence to HIPAA regulations.
Regular Audits: Implement quarterly audits of billing and coding practices to identify and rectify any discrepancies.
Operational Compliance
Comprehensive Training Program: Develop an ongoing training program for staff, focusing on compliance standards and regulatory updates.
Vendor Compliance Checks: Establish a process for regular compliance assessments of third-party vendors.
Data Security
Strengthen Cybersecurity Measures: Invest in advanced cybersecurity tools and conduct regular vulnerability assessments.
Data Backup Solutions: Implement robust data backup and recovery solutions to prevent data loss.
VI. Monitoring Plan
A continuous monitoring plan will be established to ensure the effectiveness of the implemented recommendations. This includes regular reviews of compliance metrics and ongoing staff training sessions.
VII. Conclusion
The Healthcare Compliance Risk Assessment serves as a foundational document for [Your Company Name] to proactively address compliance risks and enhance its operational integrity. By implementing the outlined recommendations, the organization can safeguard patient data and maintain compliance with healthcare regulations.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Discover peace of mind with Template.net's Healthcare Compliance Risk Assessment Template. This editable and customizable tool streamlines your compliance process, ensuring every aspect meets industry standards. Crafted with precision, it's editable in our Ai Editor Tool, empowering you to tailor assessments effortlessly. Elevate your compliance journey today with our comprehensive template.