Free SBAR Communication Nursing
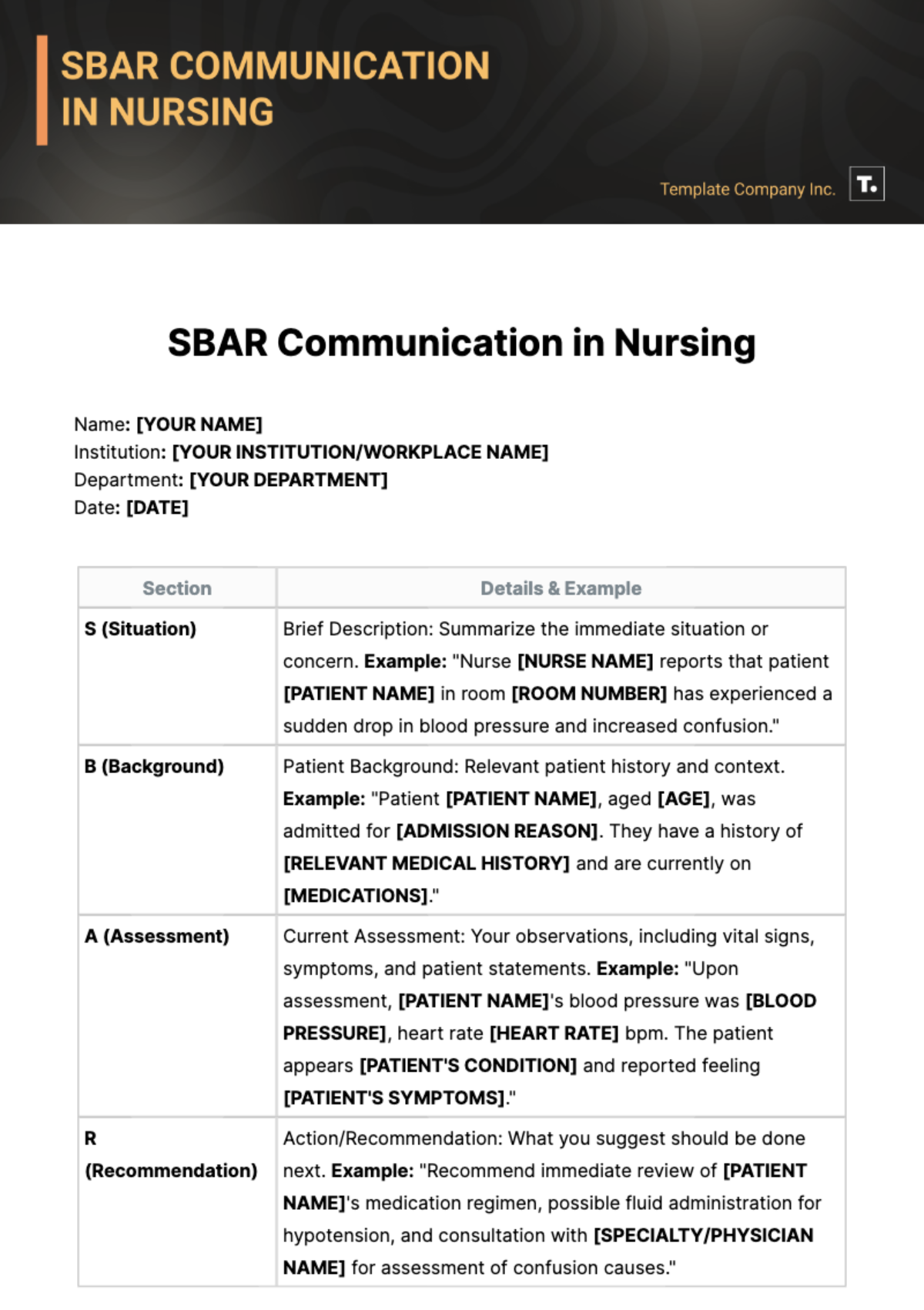
Name: [YOUR NAME]
Institution: [YOUR INSTITUTION/WORKPLACE NAME]
Department: [YOUR DEPARTMENT]
Date: [DATE]
Section | Details & Example |
|---|---|
S (Situation) | Brief Description: Summarize the immediate situation or concern. Example: "Nurse [NURSE NAME] reports that patient [PATIENT NAME] in room [ROOM NUMBER] has experienced a sudden drop in blood pressure and increased confusion." |
B (Background) | Patient Background: Relevant patient history and context. Example: "Patient [PATIENT NAME], aged [AGE], was admitted for [ADMISSION REASON]. They have a history of [RELEVANT MEDICAL HISTORY] and are currently on [MEDICATIONS]." |
A (Assessment) | Current Assessment: Your observations, including vital signs, symptoms, and patient statements. Example: "Upon assessment, [PATIENT NAME]'s blood pressure was [BLOOD PRESSURE], heart rate [HEART RATE] bpm. The patient appears [PATIENT'S CONDITION] and reported feeling [PATIENT'S SYMPTOMS]." |
R (Recommendation) | Action/Recommendation: What you suggest should be done next. Example: "Recommend immediate review of [PATIENT NAME]'s medication regimen, possible fluid administration for hypotension, and consultation with [SPECIALTY/PHYSICIAN NAME] for assessment of confusion causes." |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Discover the pinnacle of nursing communication with our SBAR Communication Nursing Template. Streamline patient care with editable and customizable templates, available for seamless integration into your workflow. Elevate efficiency and clarity in healthcare communication. Unlock the power of clear, concise documentation with Template.net. Experience intuitive editing with our Ai Editor Tool. Upgrade your nursing communication today.