Free Nursing Documentation SBAR
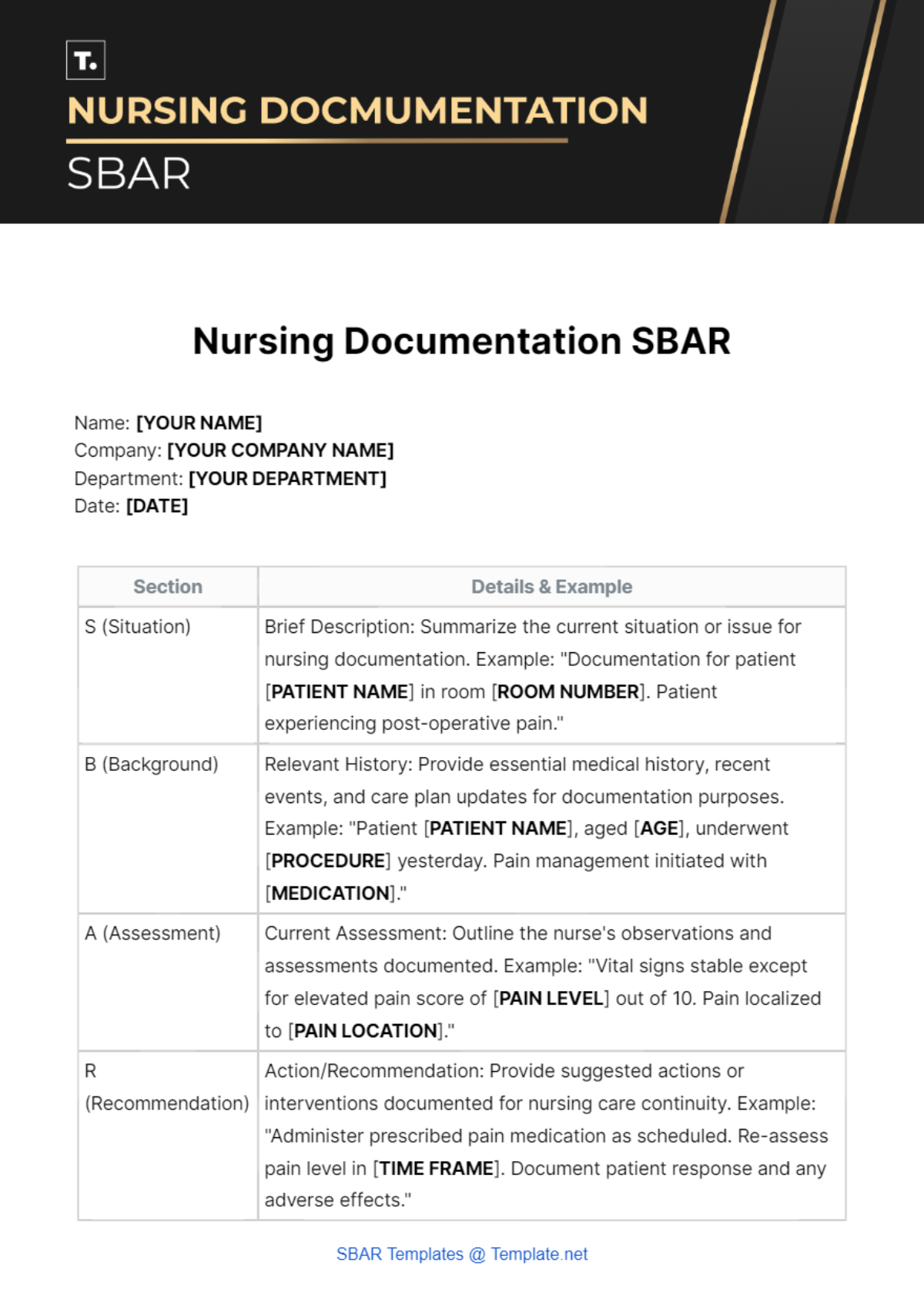
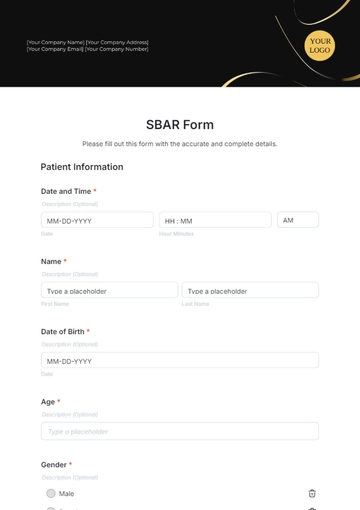
Name: [YOUR NAME]
Company: [YOUR COMPANY NAME]
Department: [YOUR DEPARTMENT]
Date: [DATE]
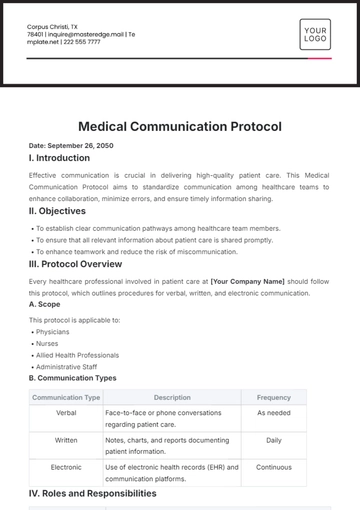
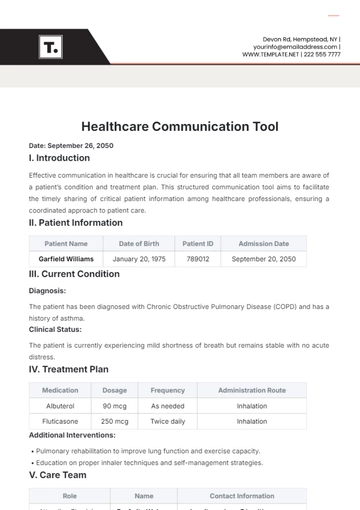
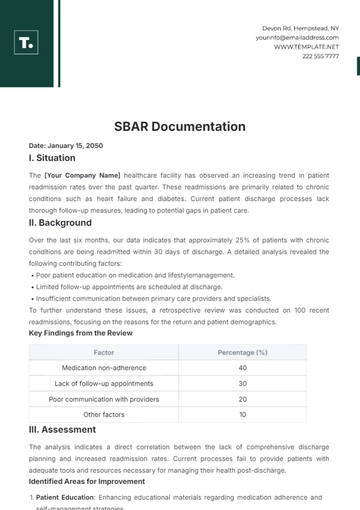
Section | Details & Example |
|---|---|
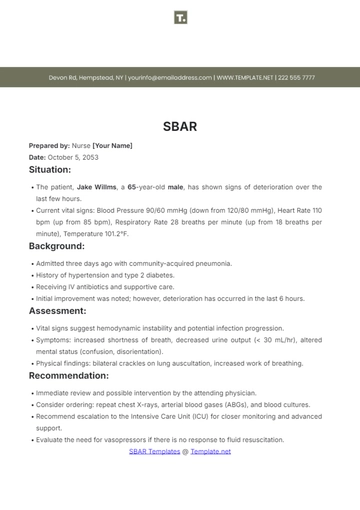
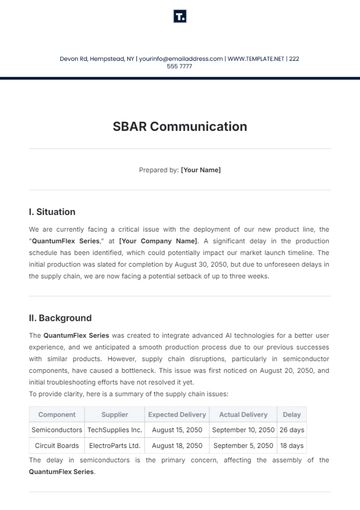
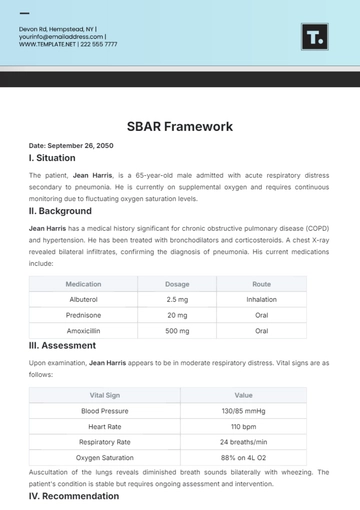
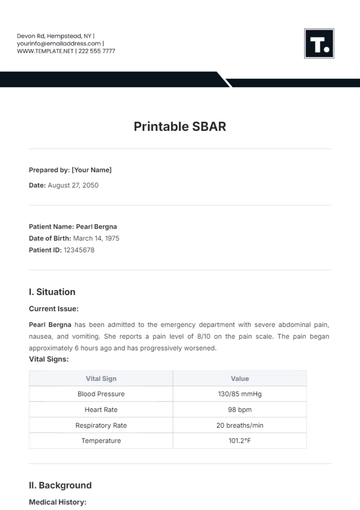
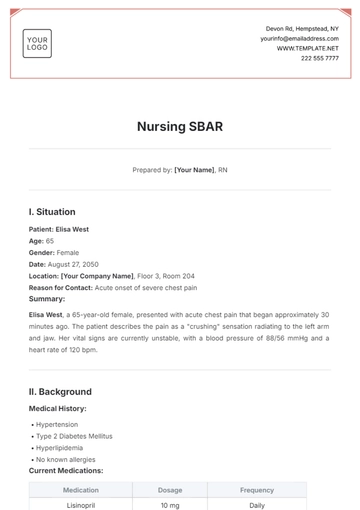
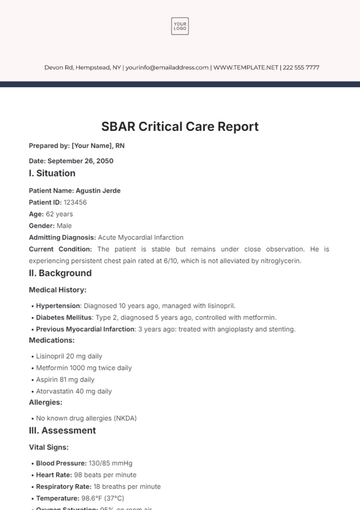
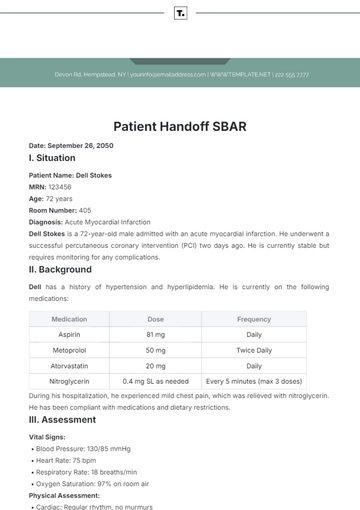
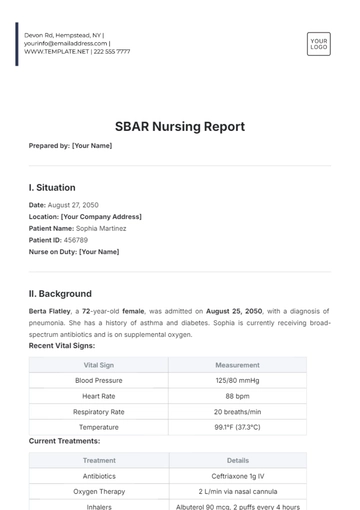
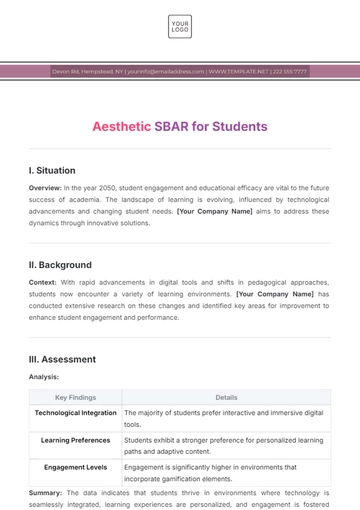
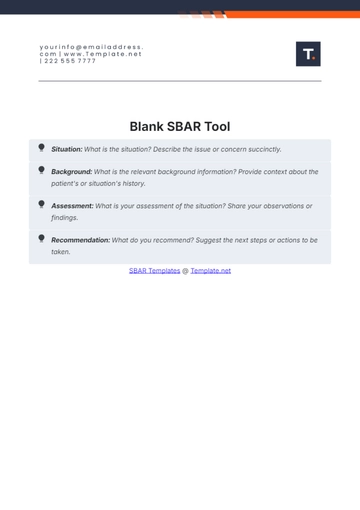
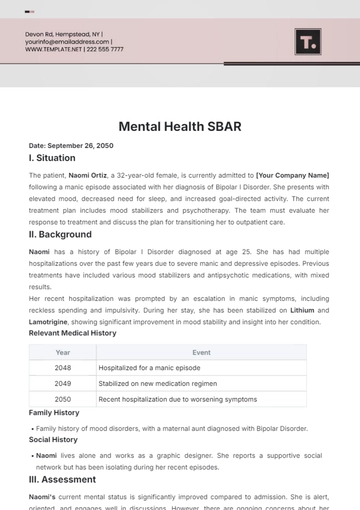
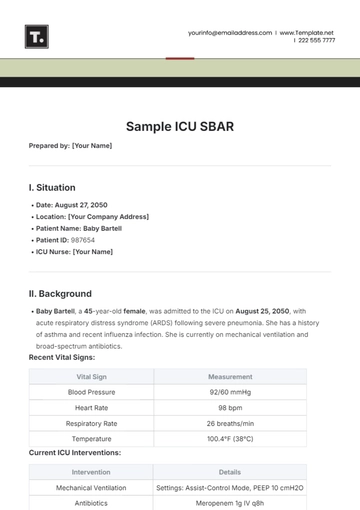
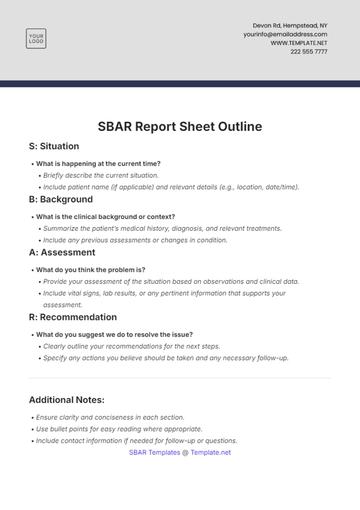
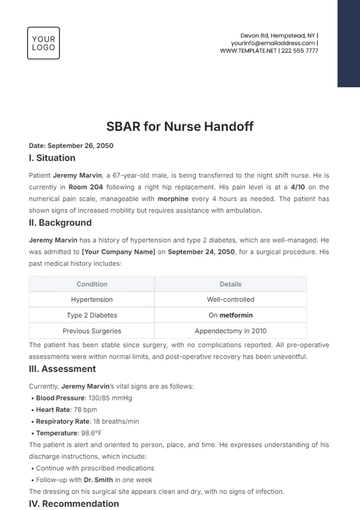
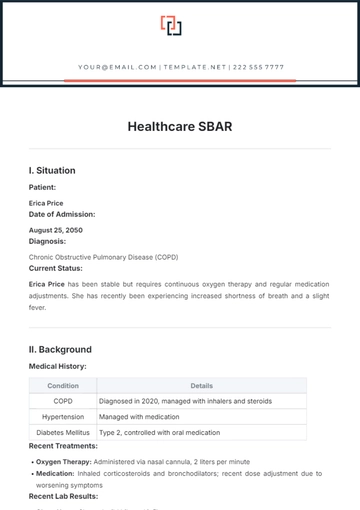
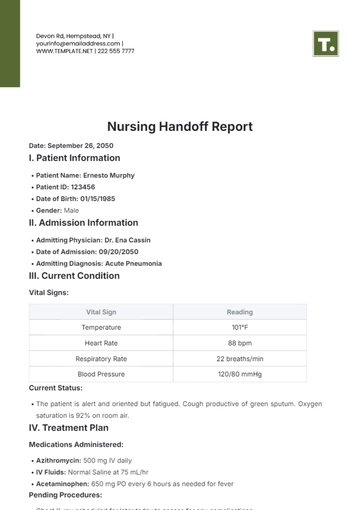
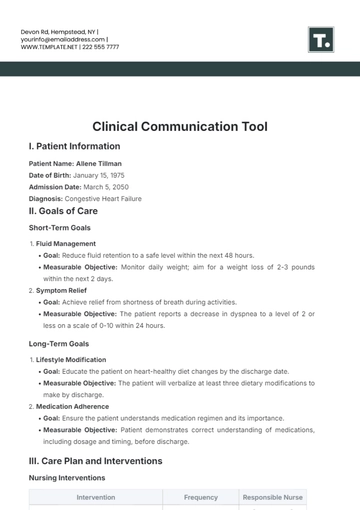
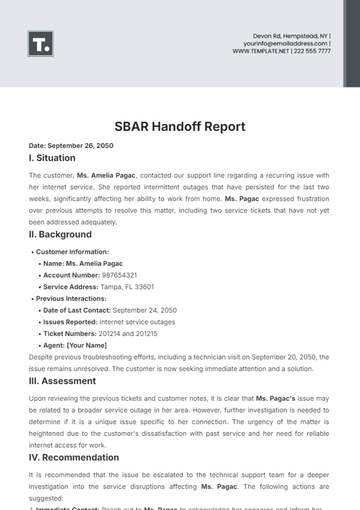
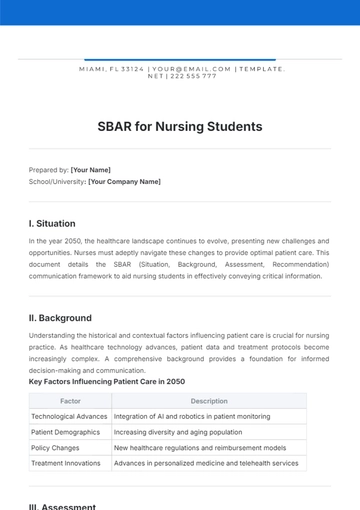
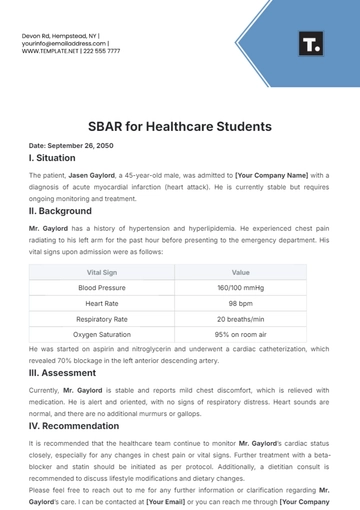
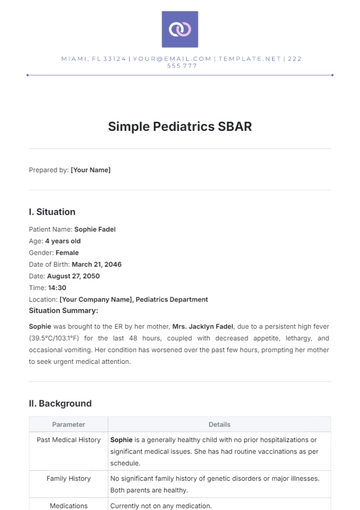
S (Situation) | Brief Description: Summarize the current situation or issue for nursing documentation. Example: "Documentation for patient [PATIENT NAME] in room [ROOM NUMBER]. Patient experiencing post-operative pain." |
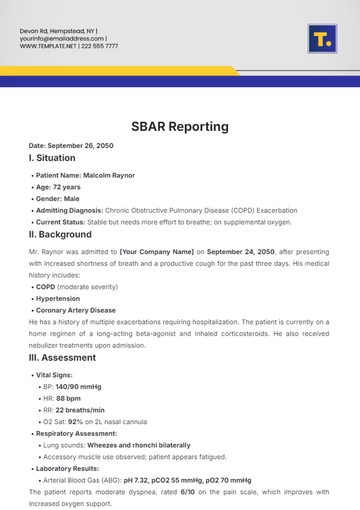
B (Background) | Relevant History: Provide essential medical history, recent events, and care plan updates for documentation purposes. Example: "Patient [PATIENT NAME], aged [AGE], underwent [PROCEDURE] yesterday. Pain management initiated with [MEDICATION]." |
A (Assessment) | Current Assessment: Outline the nurse's observations and assessments documented. Example: "Vital signs stable except for elevated pain score of [PAIN LEVEL] out of 10. Pain localized to [PAIN LOCATION]." |
R (Recommendation) | Action/Recommendation: Provide suggested actions or interventions documented for nursing care continuity. Example: "Administer prescribed pain medication as scheduled. Re-assess pain level in [TIME FRAME]. Document patient response and any adverse effects." |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing Nursing Documentation SBAR from Template.net - your ultimate solution for streamlined healthcare reporting. This editable and customizable template offers seamless integration into your workflow. Crafted for efficiency, it's editable in our Ai Editor Tool, ensuring precise communication and comprehensive documentation. Elevate your healthcare standards effortlessly.