Free Psychiatric SBAR
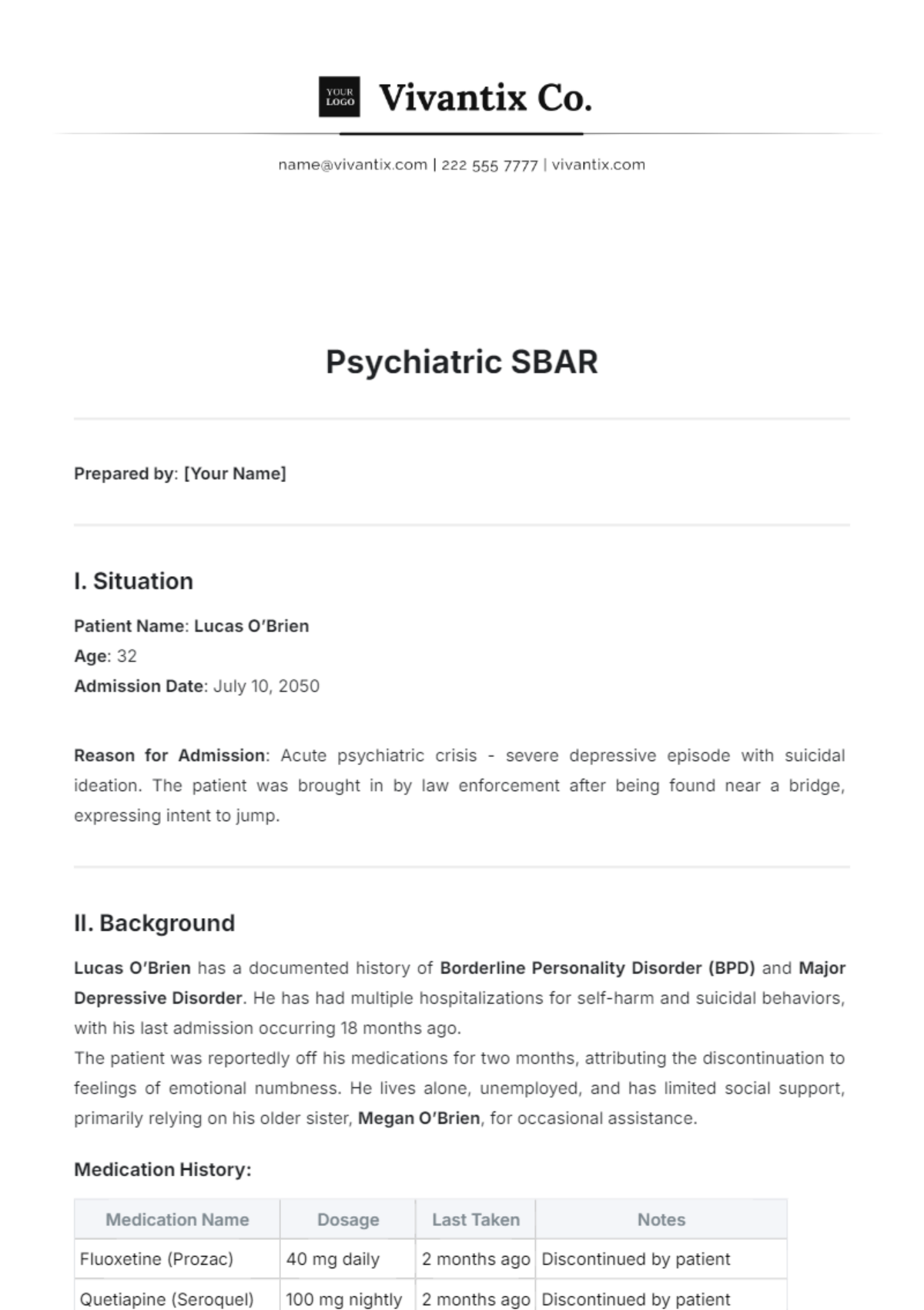
Prepared by: [Your Name]
I. Situation
Patient Name: Lucas O’Brien
Age: 32
Admission Date: July 10, 2050
Reason for Admission: Acute psychiatric crisis - severe depressive episode with suicidal ideation. The patient was brought in by law enforcement after being found near a bridge, expressing intent to jump.
II. Background
Lucas O’Brien has a documented history of Borderline Personality Disorder (BPD) and Major Depressive Disorder. He has had multiple hospitalizations for self-harm and suicidal behaviors, with his last admission occurring 18 months ago.
The patient was reportedly off his medications for two months, attributing the discontinuation to feelings of emotional numbness. He lives alone, unemployed, and has limited social support, primarily relying on his older sister, Megan O’Brien, for occasional assistance.
Medication History:
Medication Name | Dosage | Last Taken | Notes |
|---|---|---|---|
Fluoxetine (Prozac) | 40 mg daily | 2 months ago | Discontinued by patient |
Quetiapine (Seroquel) | 100 mg nightly | 2 months ago | Discontinued by patient |
Lorazepam (Ativan) PRN | 1 mg as needed | 3 months ago | Used inconsistently, per sister |
Additional Information:
Family History: Mother has untreated depression; father died by suicide at 45.
Previous Suicide Attempts: 3 documented.
Substance Use: Occasional cannabis use, denies other substances.
III. Assessment
The patient exhibits the following signs and symptoms:
Affect and Mood: Depressed mood, persistent hopelessness, significant emotional dysregulation.
Thought Process: Suicidal ideation is active but with no current plan. His thinking is ruminative and fixated on feelings of abandonment.
Insight and Judgment: Poor insight into his illness, with impaired judgment noted, particularly regarding his safety.
Behavior: Self-isolating, impulsive tendencies reported, and engagement in reckless behaviors.
Sleep and Appetite: Insomnia reported (sleeping 2-3 hours per night); decreased appetite with recent weight loss.
Cognition: Cognitive distortions present, focusing on failure and self-worthlessness.
IV. Recommendation
Immediate Safety: Continue 1:1 observation for the next 48 hours due to the high risk of suicide.
Medication Management: Restart Fluoxetine 20 mg daily and Quetiapine 50 mg nightly, gradually titrating to previous therapeutic levels over two weeks.
Therapy: Intensive dialectical behavior therapy (DBT) sessions to address emotional regulation and impulsivity, twice per week.
Family Engagement: Schedule a family meeting with Megan O’Brien to explore avenues for increased social support and monitor Lucas’ safety post-discharge.
Discharge Planning: Consider a partial hospitalization program (PHP) post-stabilization and a community-based mental health team follow-up to ensure continuity of care.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the Psychiatric SBAR Template by Template.net – your go-to resource for streamlined communication in psychiatric care. Our editable and customizable template empowers healthcare professionals to convey Situation, Background, Assessment, and Recommendation effectively. Designed for seamless integration with our AI Editor Tool, it ensures clarity and efficiency in psychiatric documentation. Simplify your workflow with Template.net.