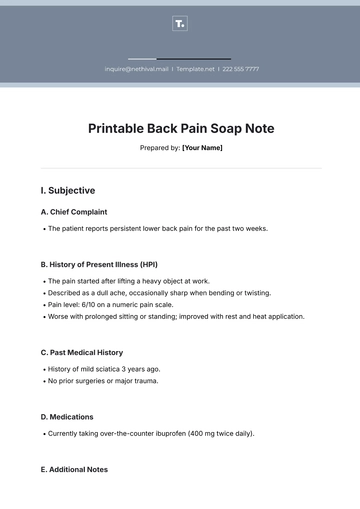
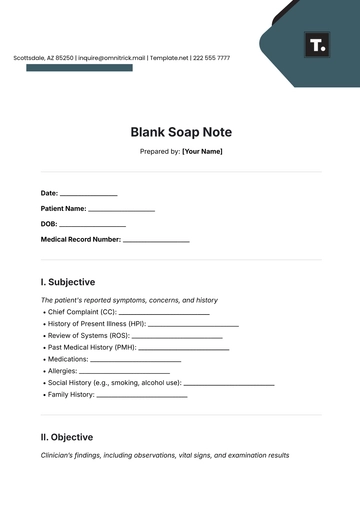
Free Printable Back Pain Soap Note
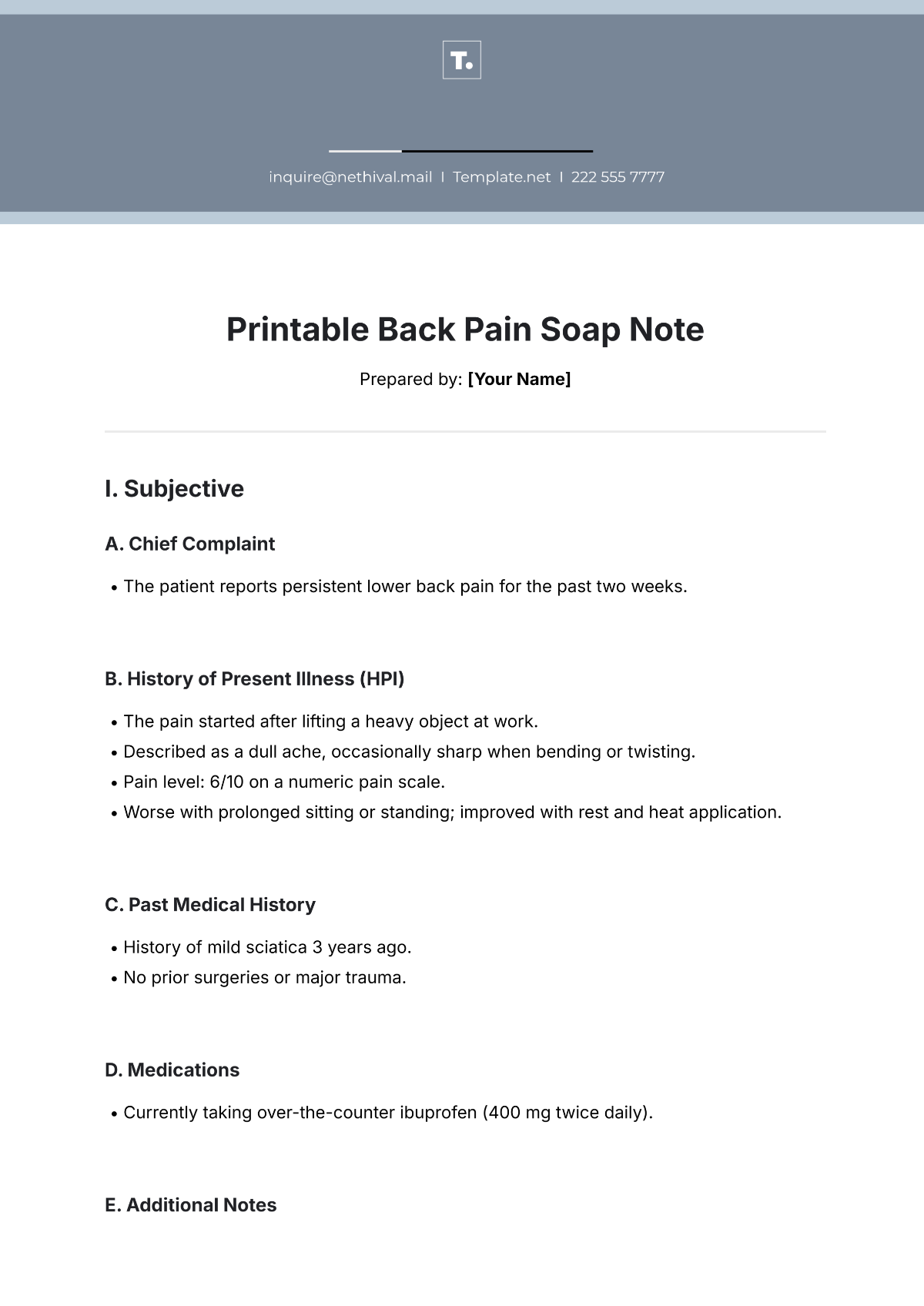
Prepared by: [Your Name]
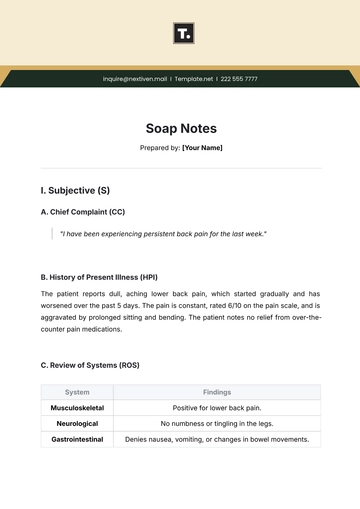
I. Subjective
A. Chief Complaint
The patient reports persistent lower back pain for the past two weeks.
B. History of Present Illness (HPI)
The pain started after lifting a heavy object at work.
Described as a dull ache, occasionally sharp when bending or twisting.
Pain level: 6/10 on a numeric pain scale.
Worse with prolonged sitting or standing; improved with rest and heat application.
C. Past Medical History
History of mild sciatica 3 years ago.
No prior surgeries or major trauma.
D. Medications
Currently taking over-the-counter ibuprofen (400 mg twice daily).
E. Additional Notes
Denies numbness, tingling, or weakness in the legs.
II. Objective
A. Physical Examination Findings
Inspection: No visible deformity or swelling in the lumbar region.
Palpation: Tenderness over the L4-L5 region; no muscle spasms noted.
Range of Motion: Limited forward flexion; extension and lateral movements are mildly painful.
Neurological Exam: Normal reflexes, muscle strength, and sensation in lower extremities.
B. Diagnostic Tests
None were conducted during this visit.
III. Assessment
A. Diagnosis
Mechanical lower back pain, likely due to muscle strain.
Rule out disc herniation or other underlying conditions.
IV. Plan
A. Treatment Recommendations
Continue ibuprofen as needed for pain relief, up to 3 times daily.
Apply a heating pad for 20 minutes, 2-3 times per day.
Avoid heavy lifting and strenuous activities for the next 1-2 weeks.
B. Therapeutic Interventions
Refer to physical therapy for strengthening exercises and posture correction.
C. Follow-Up
Reassess in two weeks or sooner if symptoms worsen.
Consider imaging (X-ray or MRI) if no improvement after four weeks.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
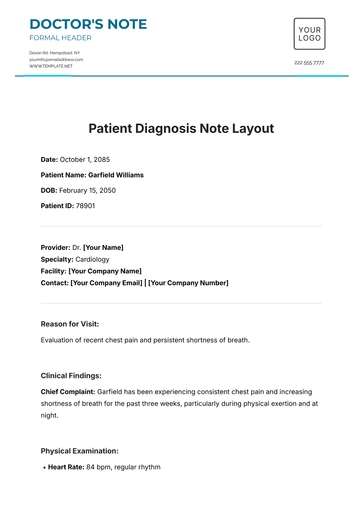
Effectively document your patient's back pain symptoms and treatment plans with our Printable Back Pain SOAP Note Template from Template.net. This fully editable and customizable template is designed to help healthcare professionals streamline their documentation process. Tailored to meet professional standards, this template allows you to effortlessly organize subjective, objective, assessment, and plan details.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note