Free Health Benefits Compliance Review HR
Introduction
A. Purpose of the Document
The purpose of this Health Benefits Compliance Review document, provided by [Your Company Name], is to ensure that our organization's health benefit programs are in full compliance with applicable laws and regulations. This document serves as a structured framework for assessing our health benefits' adherence to legal requirements and for maintaining a high standard of benefits for our employees.
B. Scope of the Review
This compliance review covers all health benefit programs offered by [Your Company Name], including medical insurance, dental coverage, vision care, and any other health-related benefits provided to our employees. The review aims to assess and maintain compliance across the entire spectrum of our health benefit offerings.
C. Document Revisions
This document is subject to periodic revisions to remain current with evolving regulations and changes in our health benefit programs. Revisions will be overseen by [Your Name] ([Your Email]) to ensure that the document reflects the most up-to-date compliance requirements.
Regulatory Framework
A. Overview of Applicable Laws and Regulations
[Your Company Name] complies with a comprehensive set of federal, state, and local laws and regulations that govern health benefit programs. These include, but are not limited to:
The Affordable Care Act (ACA)
The Employee Retirement Income Security Act (ERISA)
Health Insurance Portability and Accountability Act (HIPAA)
State-specific health benefit regulations
Understanding and adhering to these regulations is critical to maintaining compliance with health benefits. For detailed information on each regulation, please refer to the attached "Regulatory Framework" appendix.
B. Changes in Healthcare Legislation
Staying current with healthcare legislation is essential. As legislation evolves, we adapt our policies accordingly. To remain informed of changes in healthcare legislation, please visit the following resources:
Regulatory Authority 1 Website
Regulatory Authority 2 Website
[Your Company Website] - Compliance Updates
C. Contact Information for Regulatory Authorities
If you have questions or need to contact regulatory authorities for guidance or clarification, please find their contact information below:
Regulatory Authority | Contact Number |
Javier Parish | 222 555 7777 |
Solenn Williams | 222 555 7777 |
Compliance Review Checklist
A. Eligibility Criteria
To ensure compliance in this area, [Your Company Name] reviews and verifies the eligibility criteria for all employees and dependents who are eligible for our health benefit programs. The eligibility criteria are as follows:
Full-time employment status
Waiting periods
Dependent coverage requirements
Please refer to the attached "Eligibility Criteria" appendix for detailed information on eligibility criteria.
B. Coverage Provisions
Our health benefit programs are designed to provide comprehensive coverage to our employees. Key coverage provisions include:
In-network and out-of-network coverage details
Coverage limits and exclusions
Prescription drug coverage
Detailed coverage provisions can be found in the attached "Coverage Provisions" appendix.
C. Enrollment Procedures
[Your Company Name] maintains a systematic enrollment process for employees to participate in health benefit programs. The enrollment procedures include:
Enrollment periods and deadlines
Procedures for adding dependents
Electronic enrollment options
Please refer to the "Enrollment Procedures" appendix for a comprehensive overview of our enrollment process.
Documentation Review
A. Plan Documents
[Your Company Name] maintains comprehensive plan documents for each of our health benefit programs. These documents outline the terms and conditions of coverage, eligibility criteria, and other essential details. Plan documents can be accessed through [Your Company Name]'s HR portal or by contacting [Your Company Email Address].
B. Summary Plan Descriptions (SPDs)
Our Summary Plan Descriptions (SPDs) provide a concise summary of the key features of each health benefit plan offered by [Your Company Name]. SPDs are accessible to employees on our HR portal and are distributed to eligible participants upon enrollment.
C. Participant Communications
Effective communication with our employees is a priority. We regularly provide participants with important health benefit information, including plan changes, updates, and legal notices. Participants can access these communications via our company's internal communication platform.
D. Supporting Documentation
In addition to plan documents, SPDs, and participant communications, [Your Company Name] maintains various supporting documentation related to health benefit compliance. This includes records of plan amendments, IRS Form 5500 filings, and other relevant materials. These records are retained and can be accessed upon request.
Audit Process
A. Gathering Information
The audit process begins with collecting all relevant documents and data pertaining to our health benefit programs. This includes plan documents, SPDs, enrollment records, employee communications, and other compliance-related materials.
B. Assessing Compliance
Our compliance team carefully reviews the collected information to assess the extent to which our health benefit programs comply with applicable laws and regulations. This assessment includes a thorough examination of eligibility criteria, coverage provisions, enrollment procedures, and more.
C. Identifying Areas of Non-Compliance
During the assessment phase, any areas of non-compliance are identified and documented. These areas may include discrepancies in eligibility verification, inadequate disclosure, or non-adherence to nondiscrimination rules.
D. Developing Corrective Action Plans
To rectify identified non-compliance issues, [Your Company Name] develops comprehensive corrective action plans. These plans outline the specific steps and timelines required to address and remedy the non-compliance areas effectively.
E. Implementation of Corrective Actions
Upon approval of corrective action plans, [Your Company Name] takes prompt action to implement the necessary changes. This includes updating plan documents, amending procedures, and communicating changes to affected participants.
Employee Training
A. Training Programs
[Your Company Name] maintains structured training programs designed to educate employees and relevant staff members about health benefit compliance. These programs cover topics such as eligibility, enrollment procedures, and nondiscrimination rules. Training programs are accessible through [Your Company Website] - Training Portal.
B. Training Materials
In support of our training programs, we provide comprehensive training materials, including presentations, videos, and written guides. These materials are available on [Your Company Website] - Training Portal for easy access and reference.
C. Training Records
We maintain records of employee training to ensure that our staff is well-informed about health benefit compliance. Training records include details such as training dates, attendees, and topics covered. HR managers can access these records through the HR portal.
Timelines and Reporting
A. Compliance Review Schedule
[Your Company Name] conducts regular compliance reviews according to the following schedule:
Review Type | Schedule |
Annual reviews: | Annually, in January, starting from 2052 |
Quarterly reviews: | Quarterly, in March, June, September, and December, starting from 2051 |
Ad-hoc reviews: | As needed in response to regulatory changes or specific compliance concerns |
The schedule ensures that we continually monitor and maintain compliance with health benefit regulations.
B. Reporting Requirements
As part of our compliance efforts, [Your Company Name] has established reporting requirements to document and communicate compliance findings. Compliance reports must be submitted to [Your Company Email Address] by the 15th day of the month following the completion of each compliance review, starting from February 2053.
C. Recordkeeping
To meet regulatory requirements and facilitate future audits, [Your Company Name] maintains comprehensive records of compliance activities. Records are retained for a minimum of five (5) years, starting from 2050, and can be accessed through the Recordkeeping Access Portal.
Risk Assessment
A. Risk Factors
[Your Company Name] identifies several risk factors that can impact health benefit compliance, including:
Changing healthcare legislation
Evolving employee demographics
Fluctuating employee turnover rates
Complex plan designs
Regulatory penalties
These factors are considered during compliance reviews to assess potential risks accurately.
B. Prioritization of Compliance Areas
To effectively manage risks, [Your Company Name] prioritizes compliance areas based on their potential impact and likelihood of non-compliance. High-risk areas receive more frequent and thorough reviews, while lower-risk areas are assessed less frequently.
Documentation of Compliance
A. Documenting Compliance Efforts
To demonstrate our commitment to compliance, [Your Company Name] maintains detailed records of compliance efforts. These records include:
Compliance review reports
Corrective action plans
Training attendance logs
Employee communications
Regulatory updates and notifications
Documenting compliance efforts ensures transparency and provides evidence of our dedication to meeting legal requirements.
B. Record Retention
[Your Company Name] adheres to record retention policies to ensure that compliance documentation is preserved and accessible when needed. Records are retained for a minimum of seven (7) years, starting from 2055, and are stored securely on the Recordkeeping Storage System. Records may be retrieved by authorized personnel through the Record Access Process.
Conclusion
A. Summary of Findings
In summary, the Health Benefits Compliance Review conducted by [Your Company Name] has identified areas of both compliance and non-compliance within our health benefit programs. Key findings include:
Areas of Compliance:
Eligibility criteria are consistently applied.
Employee communications are clear and up-to-date.
Training programs are effective and well-documented.
Areas of Non-Compliance:
Coverage provisions require revision to align with changing regulations.
Enrollment procedures need streamlining for efficiency.
Corrective action is required to address nondiscrimination rule violations.
B. Recommendations for Ongoing Compliance
To ensure ongoing compliance and address the identified non-compliance areas, [Your Company Name] recommends the following actions:
Review and update coverage provisions in line with current regulations by June 30, 2051.
Streamline enrollment procedures for clarity and efficiency, to be completed by December 31, 2052.
Develop and implement corrective action plans to address nondiscrimination rule violations by April 15, 2053.
Conduct regular training programs for employees to ensure continued compliance awareness.
C. Contact Information for Questions or Assistance
If you have any questions or require assistance related to health benefit compliance, please feel free to reach out to our dedicated compliance team:
[Your Name] - Compliance Officer
Email: [Your Email]
Phone: [Your Phone Number]
Appendix
For more detailed information on health benefit compliance, please refer to the following appendices:
Regulatory Framework: Provides an overview of applicable laws and regulations.
Eligibility Criteria: Details the criteria for employee and dependent eligibility.
Coverage Provisions: Outlines coverage details, limits, and exclusions.
Enrollment Procedures: Describes our enrollment process and requirements.
Corrective Action Plans: Includes plans to address non-compliance issues.
Training Materials: Provides access to training presentations and resources.
Record Retention Policy: Outlines our recordkeeping and retention policy.
These appendices offer comprehensive information to support our compliance efforts.
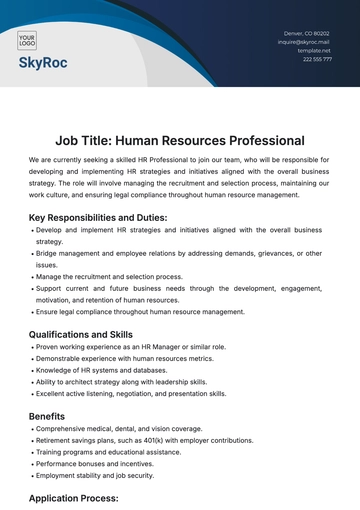
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Our Health Benefits Compliance Review Template available at Template.net is your essential tool for meticulous health benefits compliance management. Streamline eligibility checks, assess coverage provisions, and ensure disclosure adherence. Stay ahead of changing regulations, address non-compliance efficiently, and maintain comprehensive records. Elevate your health benefit programs with ease and confidence.