Free Anxiety Soap Note Professional
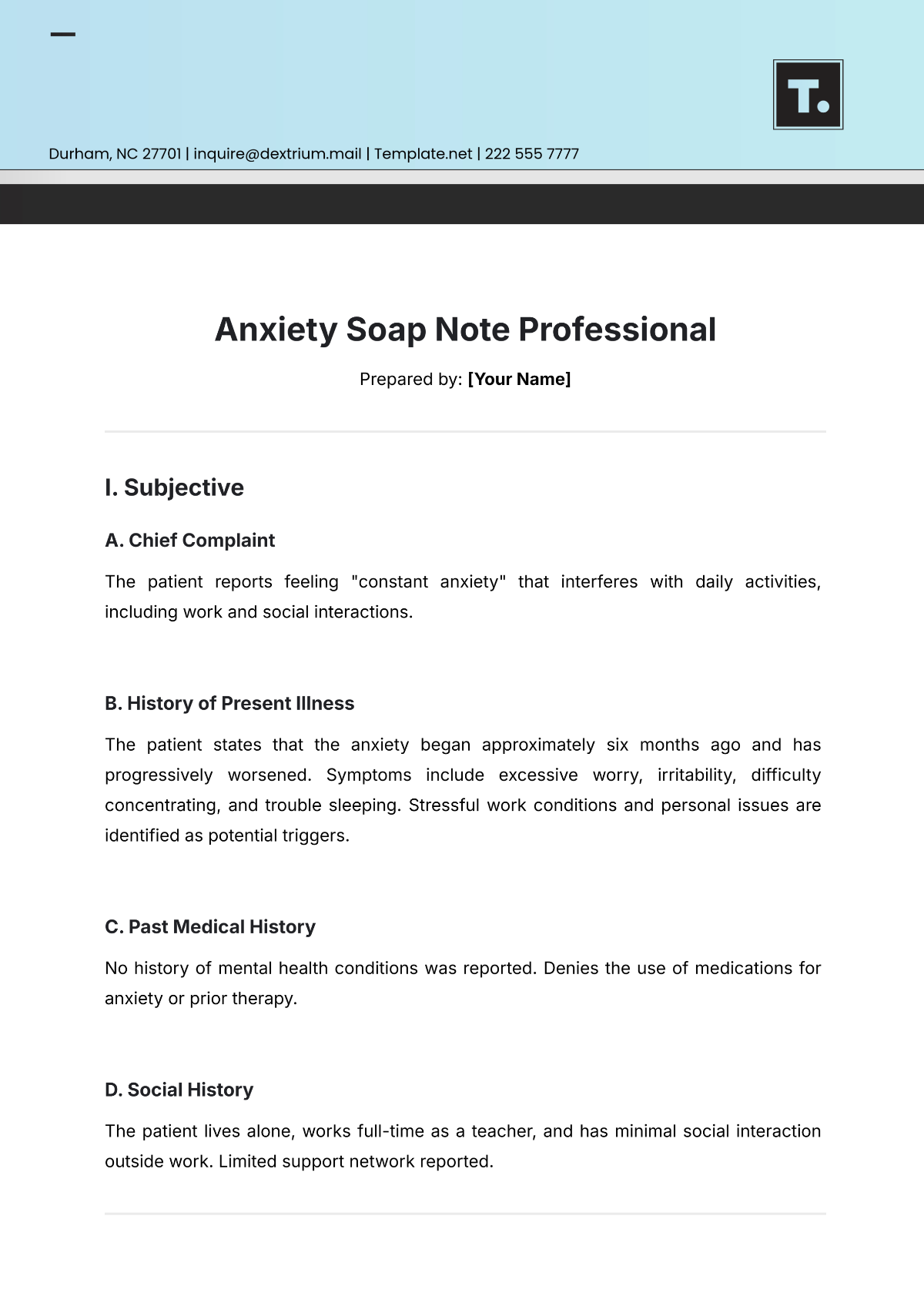
Prepared by: [Your Name]
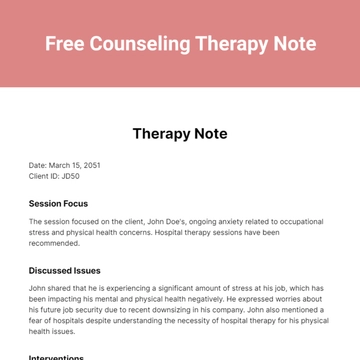
I. Subjective
A. Chief Complaint
The patient reports feeling "constant anxiety" that interferes with daily activities, including work and social interactions.
B. History of Present Illness
The patient states that the anxiety began approximately six months ago and has progressively worsened. Symptoms include excessive worry, irritability, difficulty concentrating, and trouble sleeping. Stressful work conditions and personal issues are identified as potential triggers.
C. Past Medical History
No history of mental health conditions was reported. Denies the use of medications for anxiety or prior therapy.
D. Social History
The patient lives alone, works full-time as a teacher, and has minimal social interaction outside work. Limited support network reported.
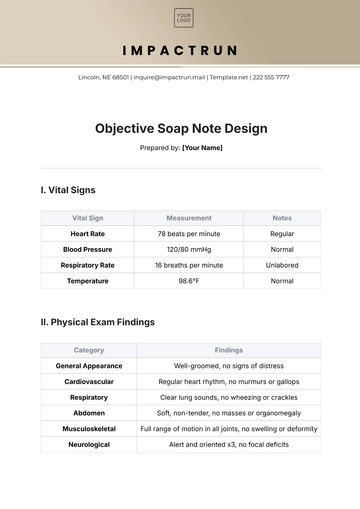
II. Objective
A. Observations | B. Vital Signs |
|---|---|
|
|
III. Assessment
A. Diagnosis
Generalized Anxiety Disorder (GAD), moderate severity, as indicated by the patient’s reported symptoms and clinical observations.
B. Clinical Summary
The patient presents with persistent anxiety and related symptoms consistent with GAD, likely exacerbated by external stressors and insufficient coping mechanisms.
IV. Plan
A. Treatment Goals
Reduce anxiety levels and improve sleep quality.
Enhance coping mechanisms for managing stress.
B. Interventions
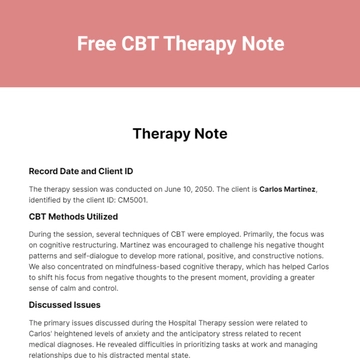
Psychotherapy: Begin cognitive-behavioral therapy (CBT) weekly for 12 weeks.
Lifestyle Modifications: Encourage regular physical activity, mindfulness exercises, and maintaining a consistent sleep schedule.
Medication Evaluation: Referral to a psychiatrist for evaluation of the need for anti-anxiety medication.
C. Follow-Up
Schedule a follow-up session in two weeks to evaluate initial progress and adjust the treatment plan as necessary.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline mental health documentation with Template.net’s Anxiety SOAP Note Professional Template. This editable and customizable template enables precise recording of subjective, objective, assessment, and plan details. Easily tailored editable in our AI Editor Tool, it ensures clarity and efficiency while meeting individual practice needs, making it a perfect tool for accurate and professional anxiety case documentation.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
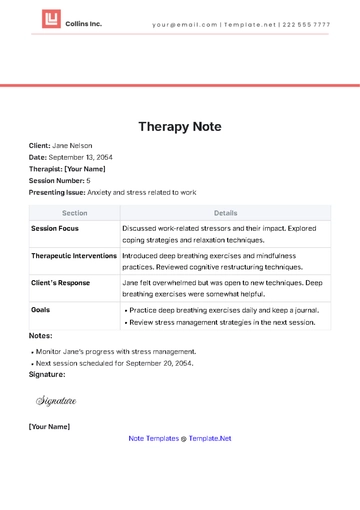
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note