Free Aesthetic Counselling Soap Note
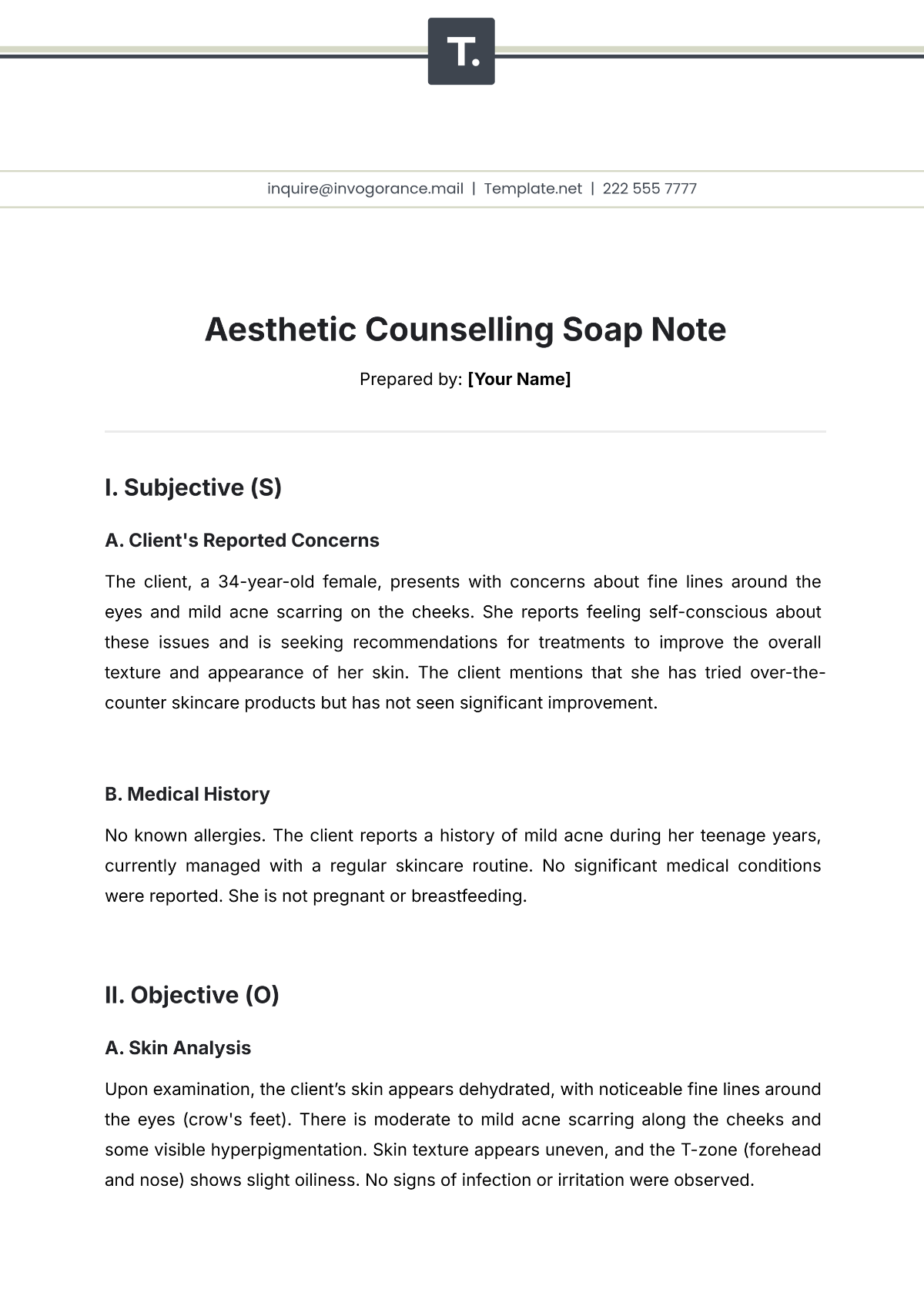
Prepared by: [Your Name]
I. Subjective (S)
A. Client's Reported Concerns
The client, a 34-year-old female, presents with concerns about fine lines around the eyes and mild acne scarring on the cheeks. She reports feeling self-conscious about these issues and is seeking recommendations for treatments to improve the overall texture and appearance of her skin. The client mentions that she has tried over-the-counter skincare products but has not seen significant improvement.
B. Medical History
No known allergies. The client reports a history of mild acne during her teenage years, currently managed with a regular skincare routine. No significant medical conditions were reported. She is not pregnant or breastfeeding.
II. Objective (O)
A. Skin Analysis
Upon examination, the client’s skin appears dehydrated, with noticeable fine lines around the eyes (crow's feet). There is moderate to mild acne scarring along the cheeks and some visible hyperpigmentation. Skin texture appears uneven, and the T-zone (forehead and nose) shows slight oiliness. No signs of infection or irritation were observed.
B. Observations
Skin tone: Mild unevenness, slight redness in the cheeks.
Skin condition: Dehydration, mild acne scarring, fine lines around the eyes.
Product usage: The client reports using daily moisturizers and serums, but no prescription or professional treatments.
III. Assessment (A)
The client’s skin condition is consistent with mild signs of aging, dehydration, and acne scarring. There are no underlying skin conditions present, but the texture and tone could benefit from targeted treatments. Fine lines around the eyes and scarring could be improved with medical-grade treatments such as chemical peels, microneedling, or hyaluronic acid-based injectables. The client’s goals are realistic, and treatments can be customized to meet her needs.
IV. Plan (P)
A. Treatment Recommendations
Hydration-focused facial: To address skin dehydration, recommend a deep hydrating facial with the use of products that include hyaluronic acid and peptides.
Microneedling: Suggest microneedling sessions to improve skin texture and reduce acne scarring. Plan for 3-4 sessions, spaced 4 weeks apart.
Topical treatments: Introduce a prescription-strength retinol product to help with fine lines and acne scars, starting at a low concentration.
Follow-up: Schedule a follow-up consultation in 6 weeks to assess progress and determine if additional treatments, such as Botox, may be necessary for the crow’s feet.
B. Education
The client was educated on proper skincare habits, including daily sunscreen use and the importance of consistency with skincare products.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Elevate your counseling documentation with our Aesthetic Counselling SOAP Note Template, exclusively at Template.net. Combining functionality and style, this editable and customizable template is perfect for recording client progress in counseling sessions. Personalize it effortlessly using our AI Editor Tool to align with your aesthetic preferences and professional requirements. Streamline your workflow while ensuring accurate, organized, and visually appealing notes.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
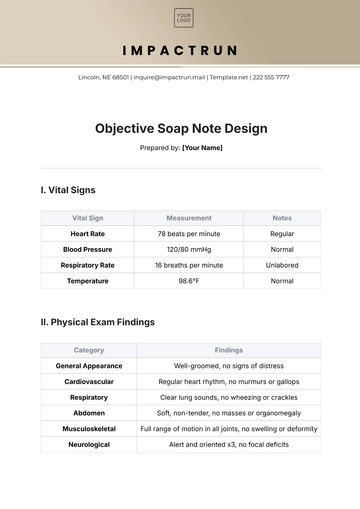
- SOAP Note Templates
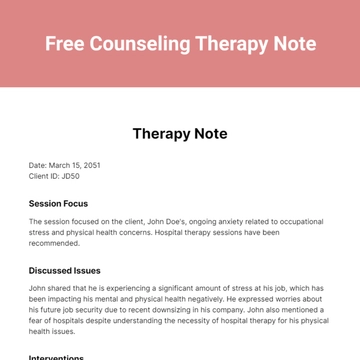
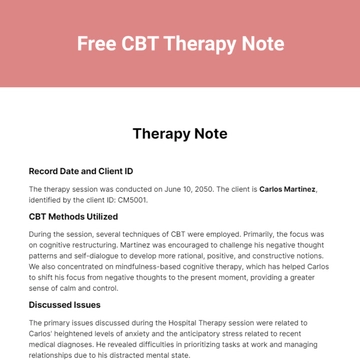
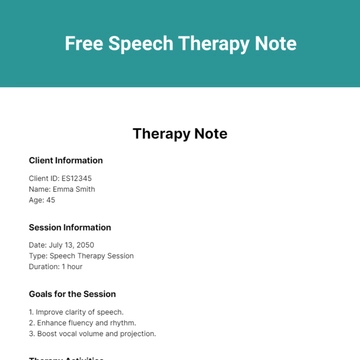
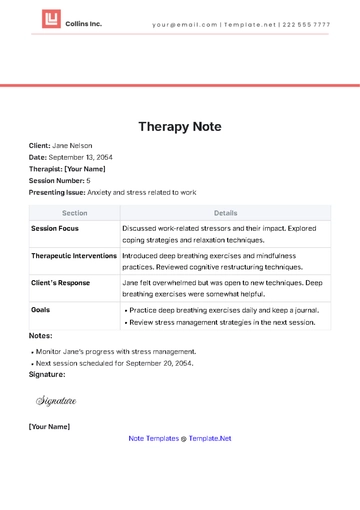
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note