Free Mental Health Soap Note
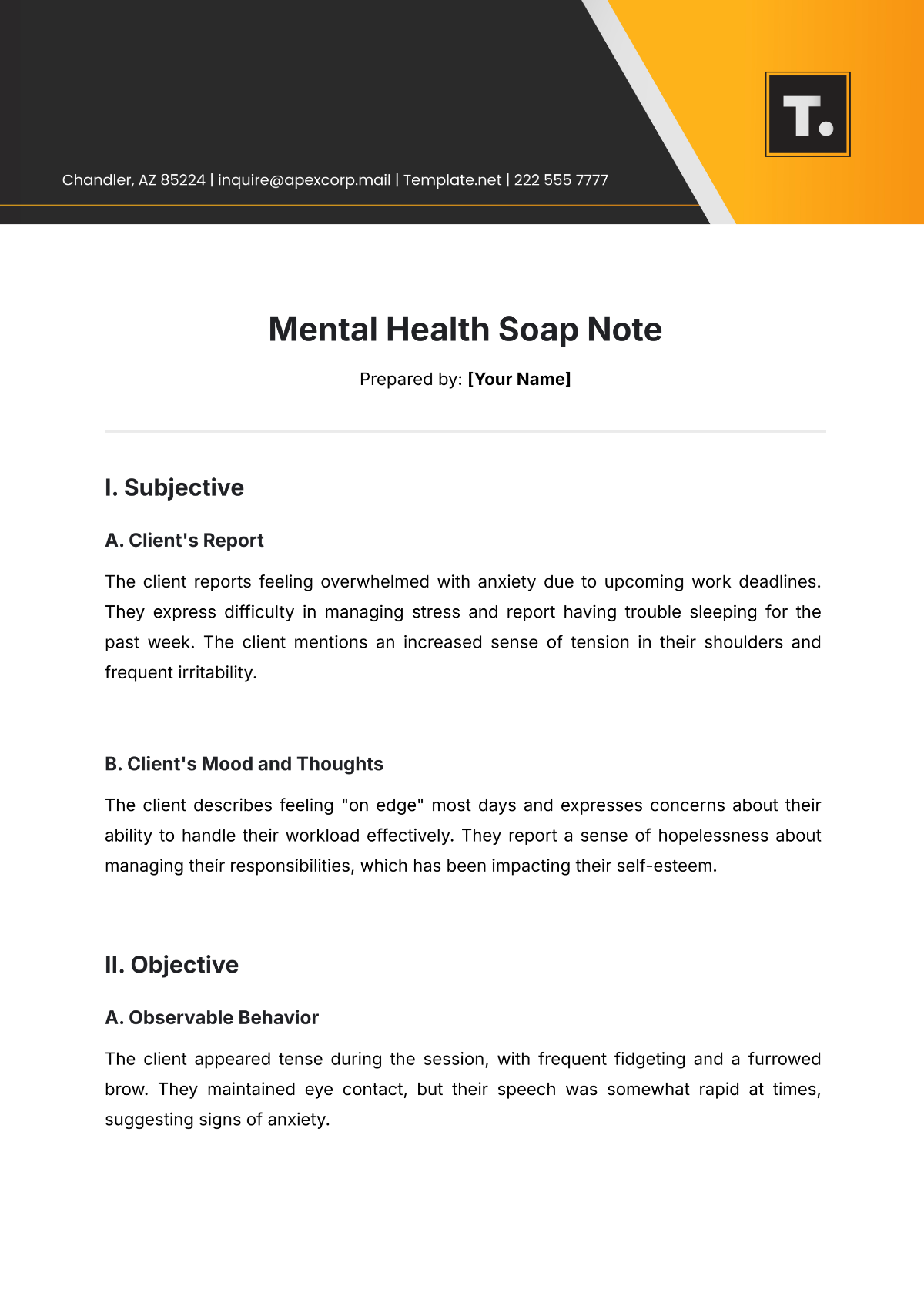
Prepared by: [Your Name]
I. Subjective
A. Client's Report
The client reports feeling overwhelmed with anxiety due to upcoming work deadlines. They express difficulty in managing stress and report having trouble sleeping for the past week. The client mentions an increased sense of tension in their shoulders and frequent irritability.
B. Client's Mood and Thoughts
The client describes feeling "on edge" most days and expresses concerns about their ability to handle their workload effectively. They report a sense of hopelessness about managing their responsibilities, which has been impacting their self-esteem.
II. Objective
A. Observable Behavior
The client appeared tense during the session, with frequent fidgeting and a furrowed brow. They maintained eye contact, but their speech was somewhat rapid at times, suggesting signs of anxiety.
B. Physical Appearance
The client was well-groomed and dressed appropriately for the session. No significant changes in appearance or hygiene were noted.
C. Clinical Data
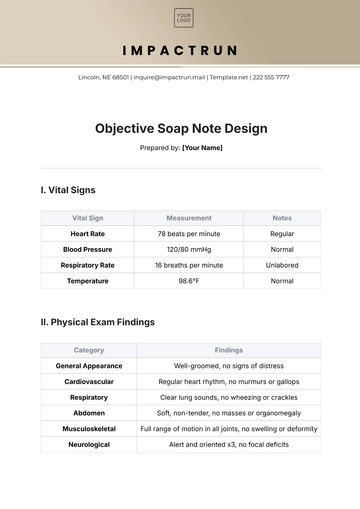
The client’s heart rate was slightly elevated at 88 beats per minute, which is higher than their normal range. Blood pressure was recorded at 132/85 mmHg, which is within the normal range but slightly elevated due to stress.
III. Assessment
The client is exhibiting signs of increased anxiety, possibly exacerbated by work-related stress. Their inability to manage stress effectively and sleep disturbances are contributing to their overall distress. The client shows a moderate level of emotional discomfort and reports a decline in their ability to cope with daily pressures.
IV. Plan
A. Treatment Goals
Focus on developing stress-management strategies, including relaxation techniques and cognitive-behavioral interventions.
Encourage regular sleep hygiene practices to improve sleep quality.
Continue to explore and challenge negative thought patterns related to work and self-worth.
B. Interventions
Introduced mindfulness breathing exercises to help with relaxation during stressful moments.
Plan to introduce Cognitive Behavioral Therapy (CBT) techniques in the next session to address anxiety triggers.
C. Next Steps
Follow-up in one week to assess progress with stress management techniques and sleep improvements. Further exploration of work-related stressors will be prioritized in the next session.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Revolutionize your mental health practice with Template.net's Mental Health Soap Note Template. This template, designed for therapists and counselors, is fully editable and customizable. It streamlines client documentation, facilitating personalized adjustments using our Ai Editor Tool, for detailed, accurate, and empathetic client care records.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note