Free Physical Therapy Soap Note
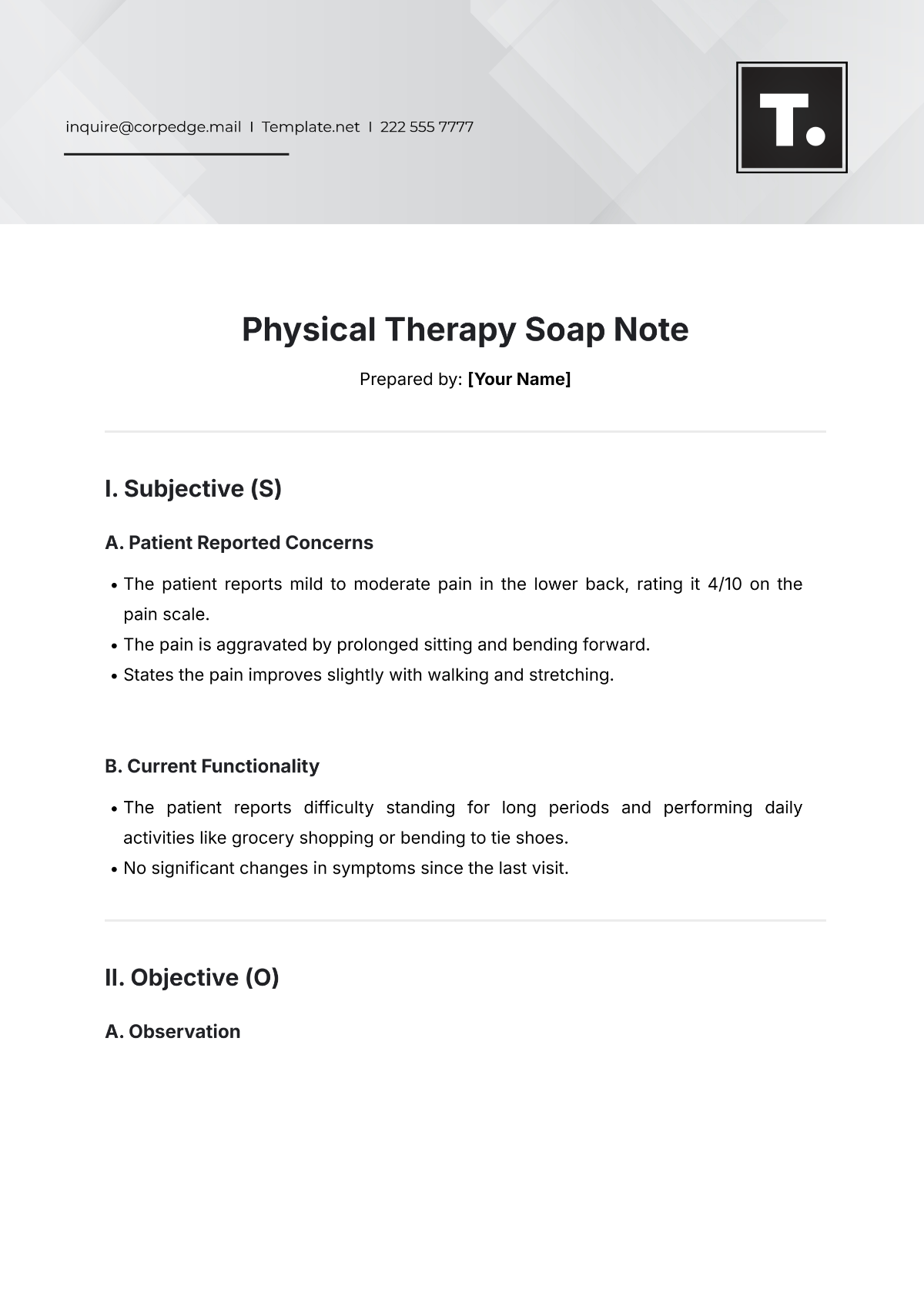
Prepared by: [Your Name]
I. Subjective (S)
A. Patient Reported Concerns
The patient reports mild to moderate pain in the lower back, rating it 4/10 on the pain scale.
The pain is aggravated by prolonged sitting and bending forward.
States the pain improves slightly with walking and stretching.
B. Current Functionality
The patient reports difficulty standing for long periods and performing daily activities like grocery shopping or bending to tie shoes.
No significant changes in symptoms since the last visit.
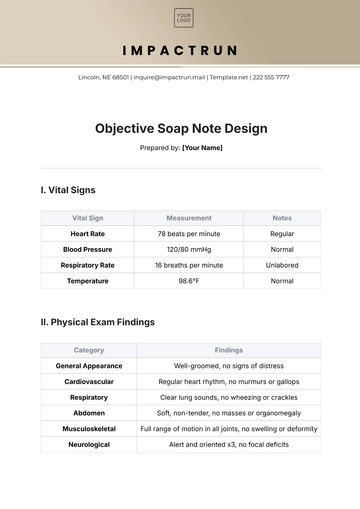
II. Objective (O)
A. Observation
Observation | Details |
|---|---|
Posture | Slight forward flexion was noted in the lumbar spine during standing |
Gait | Normal with slight favoring of the left leg |
B. Range of Motion (ROM)
Movement | Measurement | Normal Range |
|---|---|---|
Lumbar Flexion | 45° | 60° |
Lumbar Extension | 10° | 20° |
Left Hip Flexion | 90° | 110° |
C. Strength
Muscle Group | Strength Rating |
|---|---|
Lumbar extensors | 4/5 |
Left hamstring | 4/5 |
D. Special Tests
Positive straight leg raise test on the left at 45°, indicating potential nerve root involvement.
III. Assessment (A)
The patient demonstrates moderate dysfunction in lumbar mobility, particularly with flexion and extension, likely due to chronic muscle tightness and possible nerve irritation.
The reported pain level (4/10) and functional limitations indicate progress from previous visits, but more focused strengthening and stretching are needed for further improvement.
Potential need for further assessment if symptoms persist beyond the current course of therapy.
IV. Plan (P)
A. Short-Term Goals
Improve lumbar range of motion (ROM) by 10° within 2 weeks.
Decrease reported pain level to 2/10 with daily stretching and strengthening exercises.
B. Treatment Plan
Continue with manual therapy to address muscle tightness in the lumbar region.
Begin strengthening exercises for core stabilization (e.g., bridges, planks) and hamstring stretches.
Reassess functional mobility at the next session to adjust the treatment plan if necessary.
C. Patient Education
Instruct patient on proper posture while sitting and standing to reduce strain on the lumbar spine.
Recommend a home exercise program including daily stretches for the lower back and hamstrings.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Advance patient care with Template.net's Physical Therapy Soap Note Template. Designed for physical therapists, this editable, customizable tool is key for precise treatment documentation. Modify it to suit individual patient needs using our Ai Editor Tool, ensuring detailed, accurate therapy records for optimal rehabilitation outcomes.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
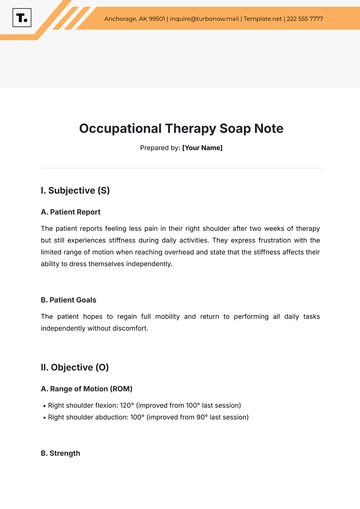
- SOAP Note Templates
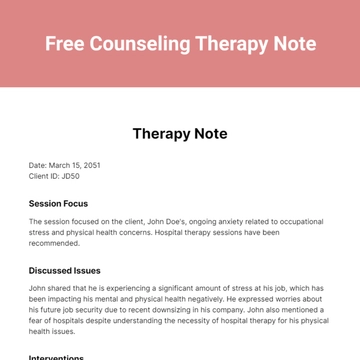
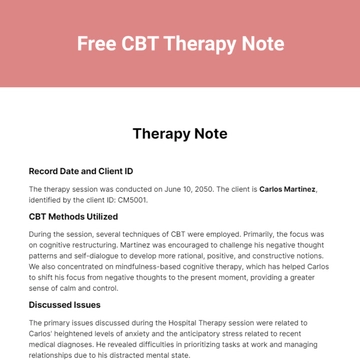
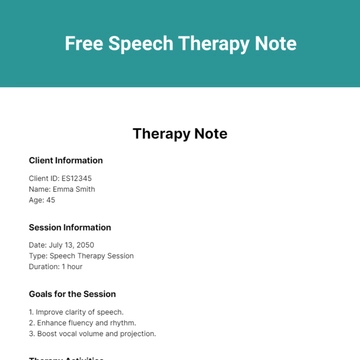
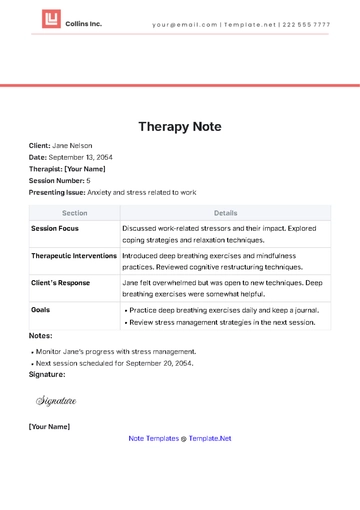
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note