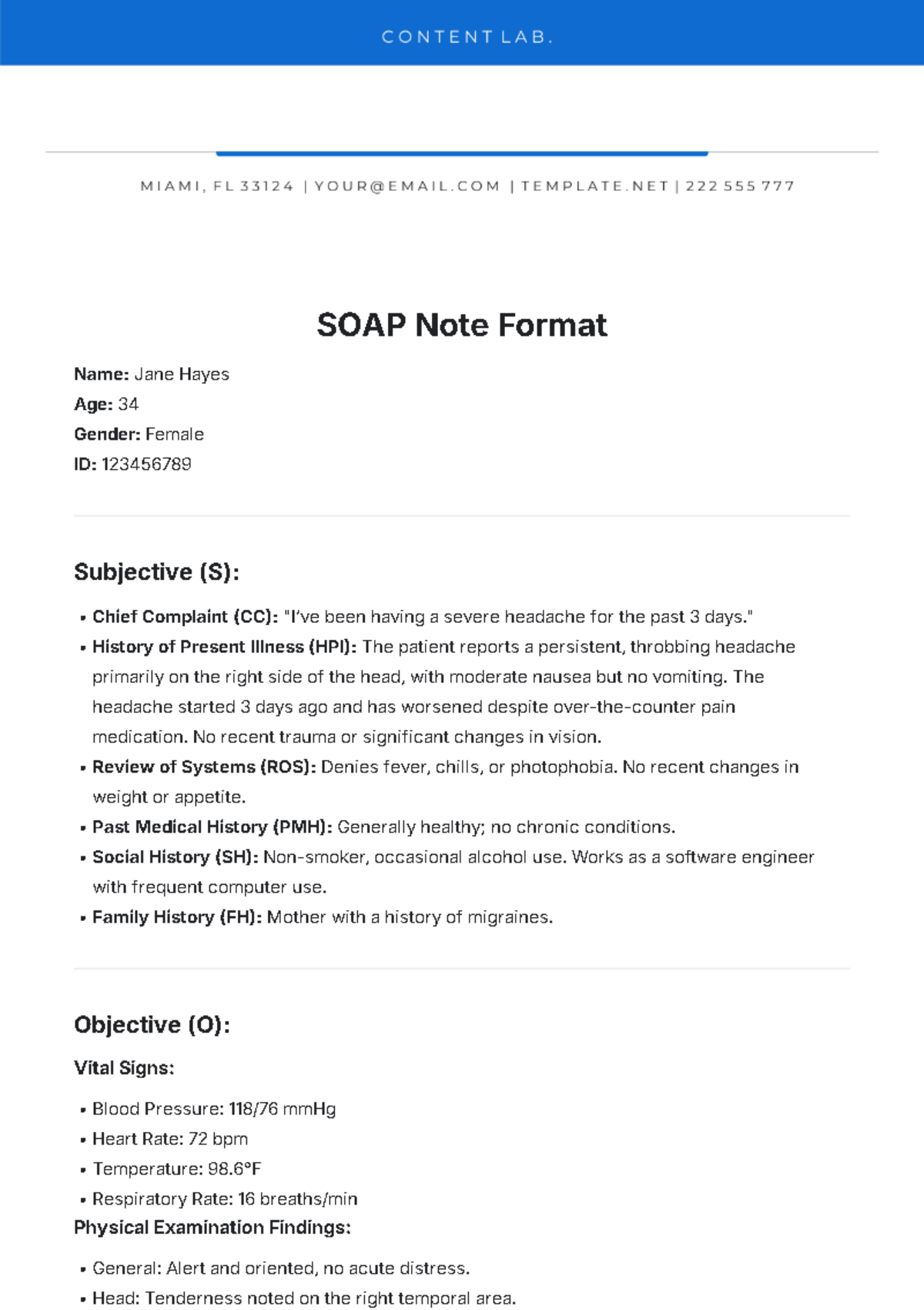
Free SOAP Note Format
Prepared by: [Your Name]
I. Subjective
A. Chief Complaint (CC)
The primary reason for the patient's visit is expressed in their own words.
Example: "I have been experiencing severe headaches for the past three days."
B. History of Present Illness (HPI)
Details about the onset, duration, intensity, and factors affecting the patient's symptoms.
Example: Headaches began three days ago, worsen with bright lights, and improve slightly with rest.
C. Past Medical History (PMH)
Relevant medical history, including chronic conditions, past surgeries, or hospitalizations.
Example: History of migraines and hypertension.
D. Medications
Current medications the patient is taking, including dosages and frequency.
Example: Lisinopril 10 mg daily, ibuprofen as needed.
E. Allergies
Known allergies to medications, foods, or environmental factors.
Example: Allergic to penicillin.
F. Family and Social History
Relevant family medical history and lifestyle factors.
Example: Family history of migraines; patient smokes one pack of cigarettes daily.
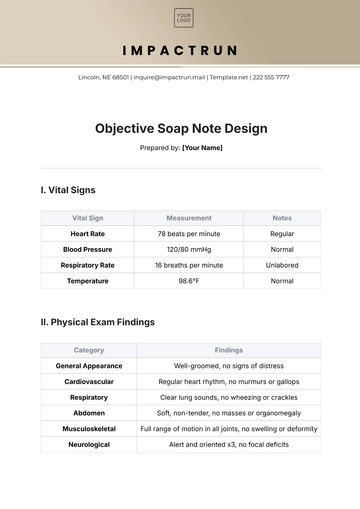
II. Objective
A. Vital Signs
Document measurable data such as blood pressure, heart rate, respiratory rate, and temperature.
Example: BP: 140/90 mmHg, HR: 80 bpm, Temp: 98.6°F.
B. Physical Examination
Findings from the healthcare provider's examination of the patient.
Example: No neurological deficits noted; tenderness in the forehead region.
C. Laboratory and Diagnostic Results
Relevant test results or imaging findings.
Example: Normal CT scan; elevated white blood cell count.
III. Assessment
A. Diagnosis or Clinical Impression
The healthcare provider’s interpretation of the data collected.
Example: Tension headache possibly exacerbated by stress and poor sleep habits.
IV. Plan
A. Treatment Plan
Details about the prescribed treatment or intervention.
Example: Prescribe acetaminophen 500 mg as needed for pain; recommend relaxation techniques.
B. Follow-Up Instructions
Guidance for the patient on next steps or scheduled check-ups.
Example: Follow up in one week if symptoms persist or worsen.
C. Referrals
Recommendations for specialist consultations, if necessary.
Example: Refer to a neurologist for further evaluation.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Transform patient care documentation with Template.net's Soap Note Template. Expertly crafted for healthcare professionals, this editable and customizable template streamlines note-taking. Easily adapt it to specific patient needs using our Ai Editor Tool, ensuring accurate and efficient record-keeping for optimal patient care.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
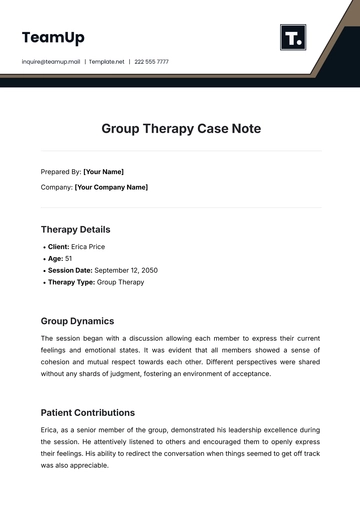
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
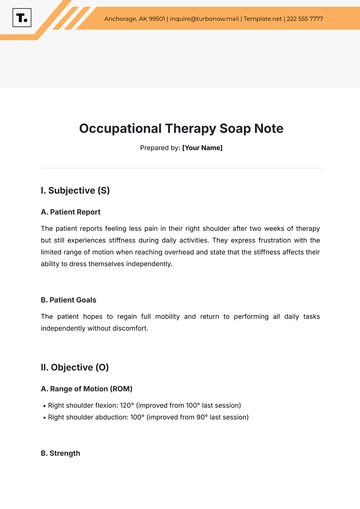
- SOAP Note Templates
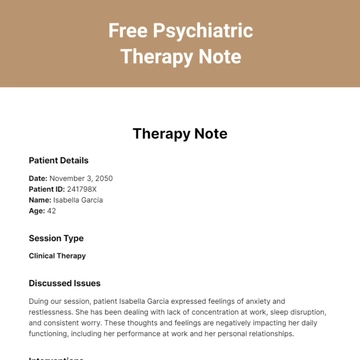
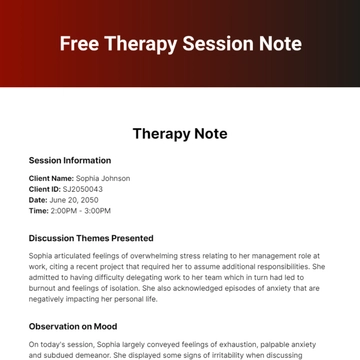
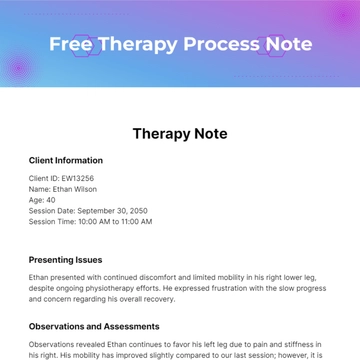
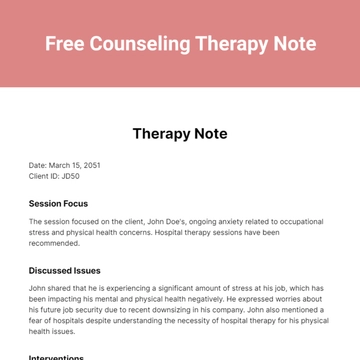
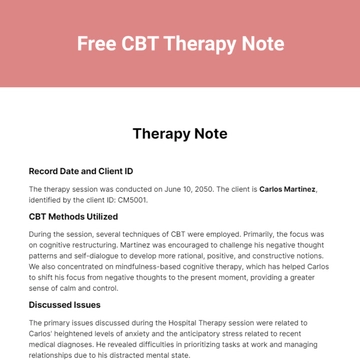
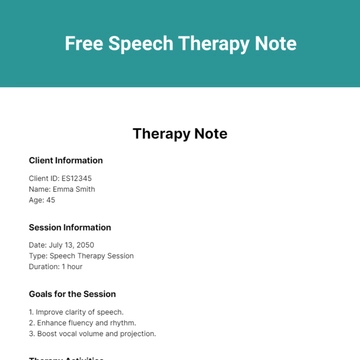
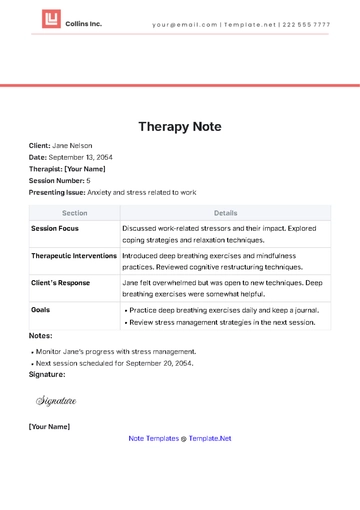
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note