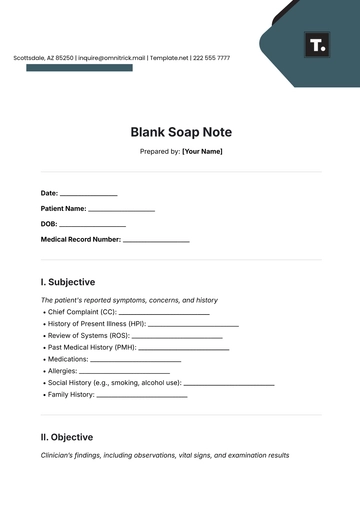
Free Blank Soap Note
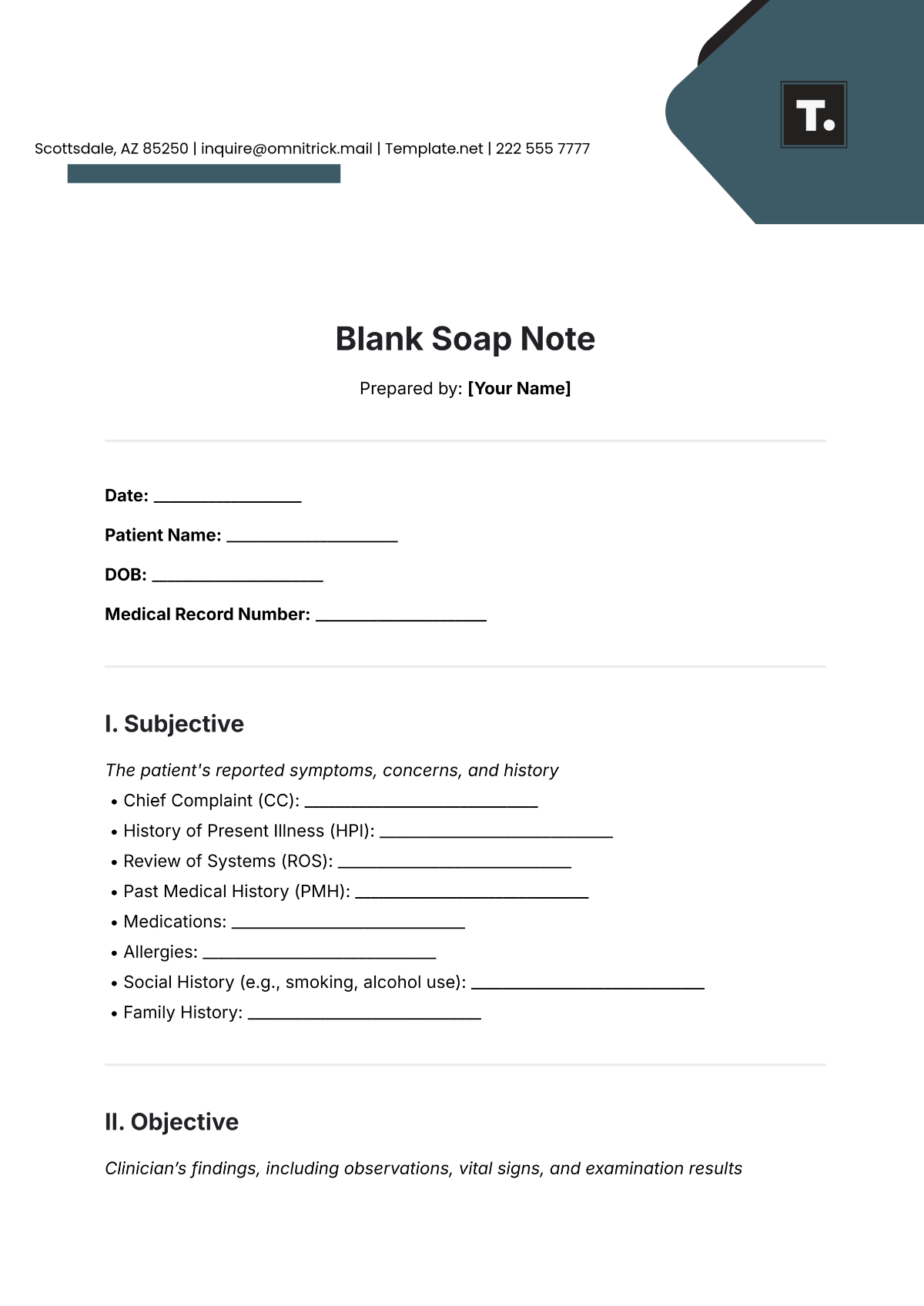
Prepared by: [Your Name]
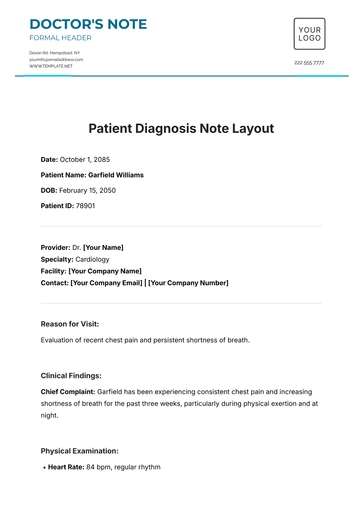
Date: ___________________
Patient Name: ______________________
DOB: ______________________
Medical Record Number: ______________________
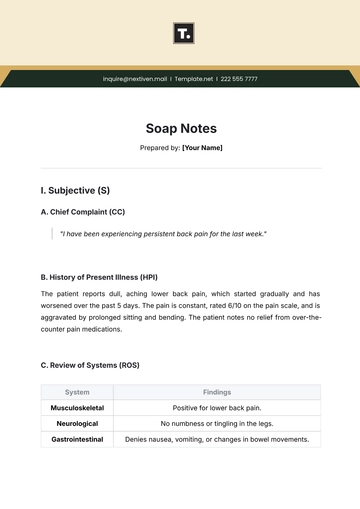
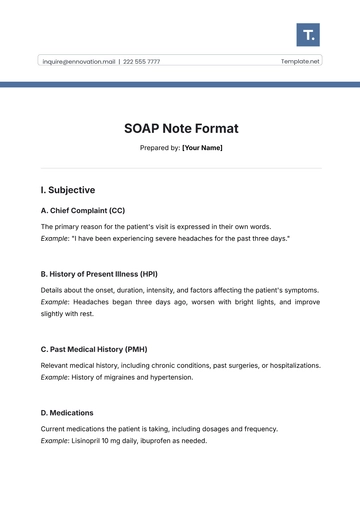
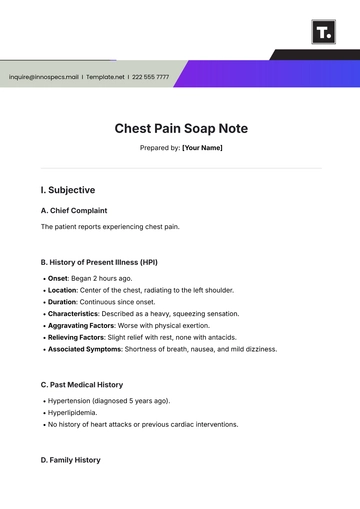
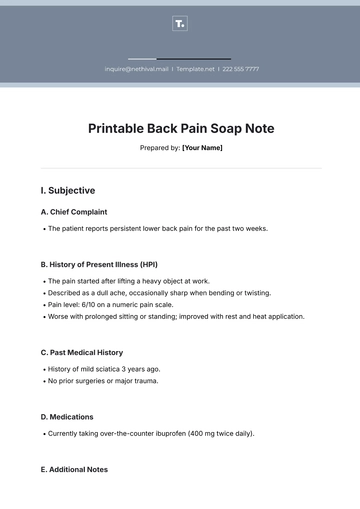
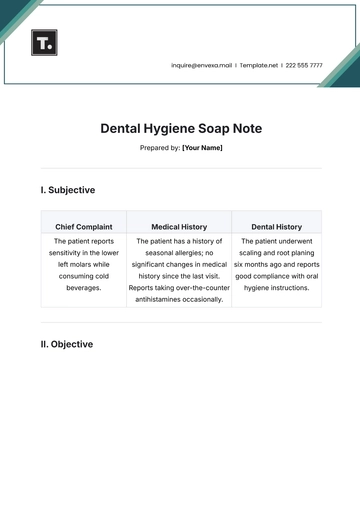
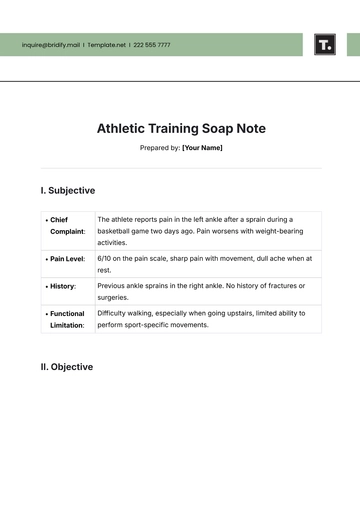
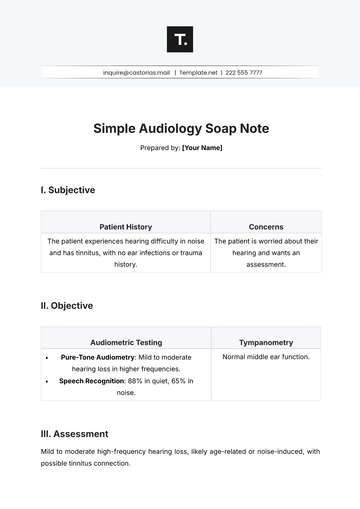
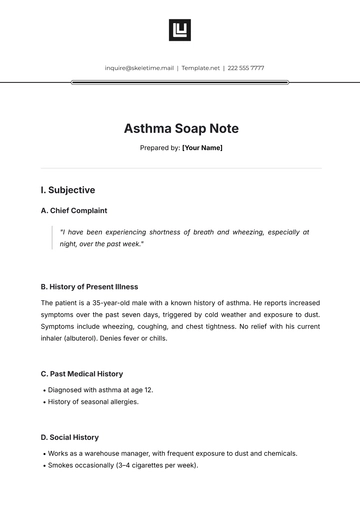
I. Subjective
The patient's reported symptoms, concerns, and history
Chief Complaint (CC): ______________________________
History of Present Illness (HPI): ______________________________
Review of Systems (ROS): ______________________________
Past Medical History (PMH): ______________________________
Medications: ______________________________
Allergies: ______________________________
Social History (e.g., smoking, alcohol use): ______________________________
Family History: ______________________________
II. Objective
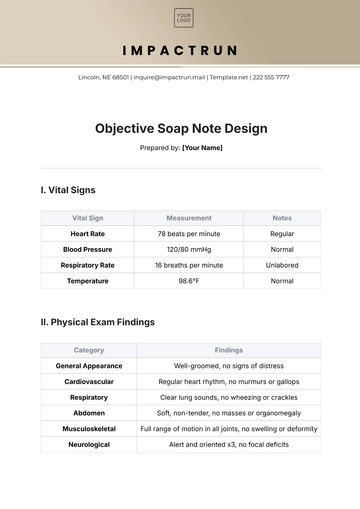
Clinician’s findings, including observations, vital signs, and examination results
Vital Signs:
Temperature: __________
Pulse: __________
Blood Pressure: __________
Respiratory Rate: __________
Oxygen Saturation: __________
Physical Exam:
General Appearance: ______________________________
HEENT (Head, Eyes, Ears, Nose, Throat): ______________________________
Cardiovascular: ______________________________
Respiratory: ______________________________
Abdominal: ______________________________
Musculoskeletal: ______________________________
Neurological: ______________________________
Laboratory/Diagnostic Results: ______________________________
Imaging: ______________________________
III. Assessment
Clinician’s interpretation based on subjective and objective data
Diagnosis/Clinical Impression: ______________________________
Differential Diagnosis: ______________________________
Severity: ______________________________
IV. Plan
Plan of action for further management
Treatment: ______________________________
Medications: ______________________________
Tests/Labs: ______________________________
Referrals: ______________________________
Follow-up: ______________________________
Patient Education: ______________________________

Name of Clinician: ______________________
Title: ______________________
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Discover the efficiency of clinical documentation with Template.net's Blank Soap Note Template. Exclusively designed for healthcare professionals, this template is fully editable and customizable. Perfect for patient records, it's easily tailored to specific needs using our advanced Ai Editor Tool, ensuring accuracy and clarity in every entry.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note