Free Primary Care Soap Note
Patient Information
Name: Tom Walter
Age: 45
Gender: Male
Date: November 26, 2050
Reason for Visit: Annual check-up and evaluation of hypertension
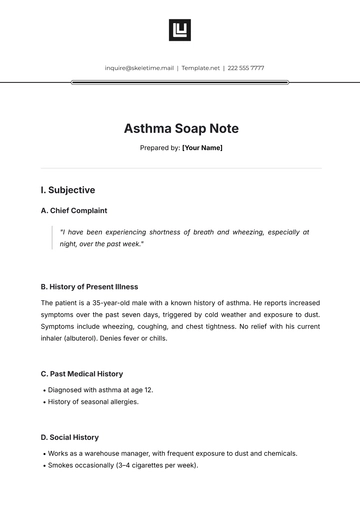
I. Subjective
A. Chief Complaint
"I came in for my annual check-up and would like to make sure my blood pressure is under control."
B. History of Present Illness
Tom reports that he has a history of high blood pressure, which has been managed with medication for the past 2 years. He states that he feels well overall, with no chest pain or shortness of breath. He has been following a low-salt diet and exercising regularly. No recent changes in weight, diet, or lifestyle.
C. Review of Systems
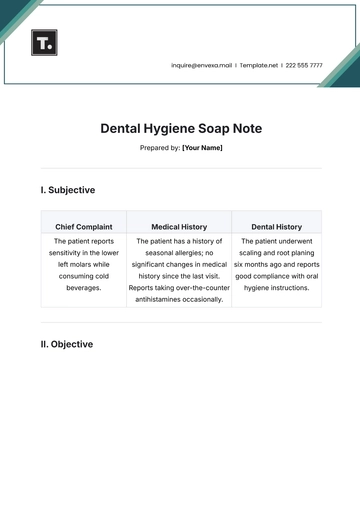
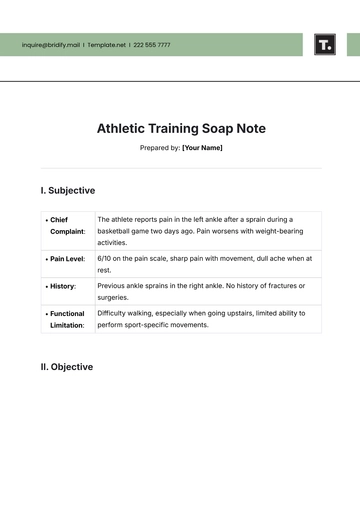
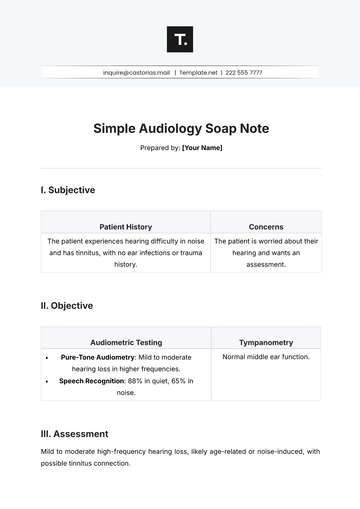
System | Findings |
|---|---|
Cardiovascular | No palpitations or chest pain. |
Respiratory | No shortness of breath, cough, or wheezing. |
Gastrointestinal | No nausea, vomiting, or abdominal pain. |
Musculoskeletal | No joint pain or stiffness. |
Neurological | No headaches, dizziness, or visual disturbances. |
D. Medications
Lisinopril 10 mg daily, aspirin 81 mg daily.
E. Allergies
No known drug allergies.
II. Objective
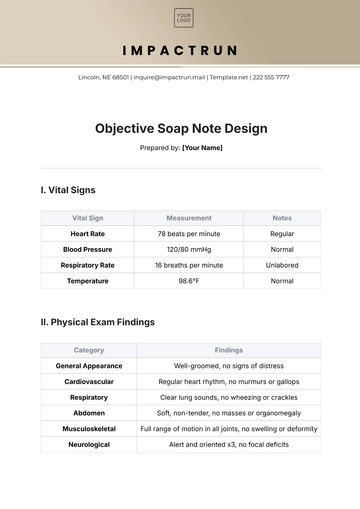
A. Vital Signs
Vital Sign | Value |
|---|---|
Blood Pressure | 138/85 mmHg (left arm, seated) |
Heart Rate | 72 bpm |
Respiratory Rate | 16 breaths/min |
Temperature | 98.4°F (oral) |
Weight | 210 lbs |
Height | 5'10" |
B. Physical Exam
System | Findings |
|---|---|
General | Alert and oriented, in no acute distress. |
Cardiovascular | Regular rate and rhythm, no murmurs or gallops. |
Respiratory | Clear to auscultation bilaterally. |
Gastrointestinal | Abdomen soft, non-tender, no hepatosplenomegaly. |
Musculoskeletal | Full range of motion, no joint deformities. |
Neurological | Cranial nerves intact, normal gait, no focal deficits. |
III. Assessment
Hypertension is well-controlled on current medication.
No evidence of acute illness or complications.
The patient is at risk for developing complications if blood pressure remains uncontrolled.
IV. Plan
Continue current medication regimen (Lisinopril 10 mg daily).
Advise regular monitoring of blood pressure at home.
Encourage weight loss, continued exercise, and a low-sodium diet.
Follow-up appointment in 6 months for blood pressure recheck.
Discuss lifestyle modifications to further reduce cardiovascular risk.
Educate the patient about symptoms of hypertension complications (e.g., chest pain, dizziness).
Signature

Dr. [Your Name], MD
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Elevate primary care with Template.net's Primary Care Soap Note Template. Expertly crafted for medical practitioners, this editable and customizable template is a game-changer. It simplifies patient documentation, making it easily adaptable for individual cases with our Ai Editor Tool, ensuring precise and efficient patient care records.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note