Free Sample Soap Note
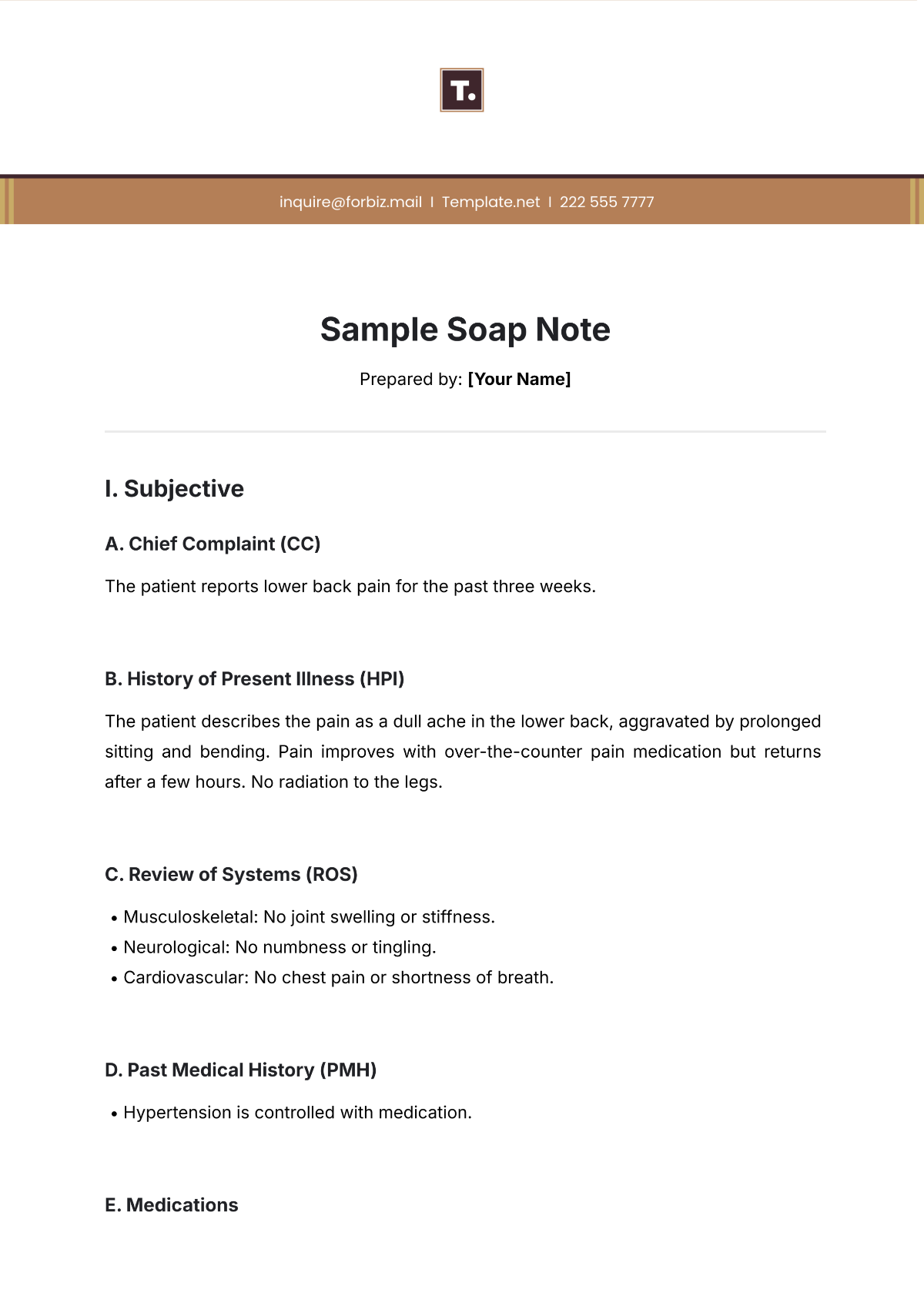
Prepared by: [Your Name]
I. Subjective
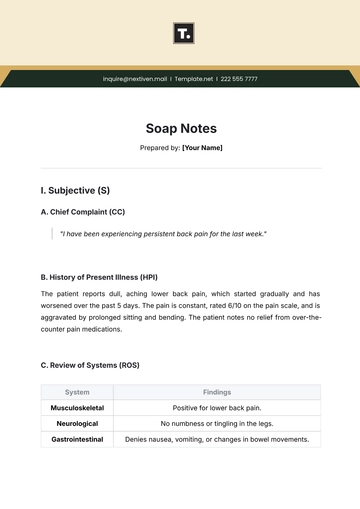
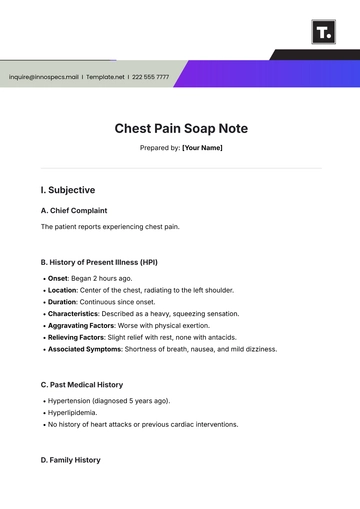
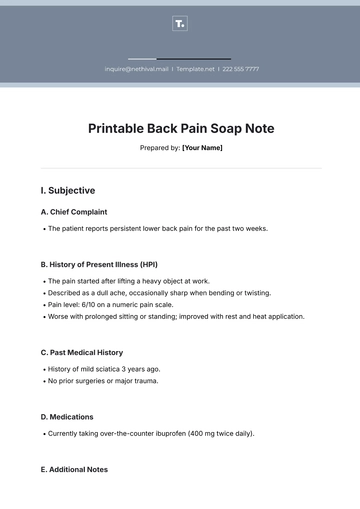
A. Chief Complaint (CC)
The patient reports lower back pain for the past three weeks.
B. History of Present Illness (HPI)
The patient describes the pain as a dull ache in the lower back, aggravated by prolonged sitting and bending. Pain improves with over-the-counter pain medication but returns after a few hours. No radiation to the legs.
C. Review of Systems (ROS)
Musculoskeletal: No joint swelling or stiffness.
Neurological: No numbness or tingling.
Cardiovascular: No chest pain or shortness of breath.
D. Past Medical History (PMH)
Hypertension is controlled with medication.
E. Medications
Lisinopril 10 mg daily.
F. Allergies
No known drug allergies.
G. Family History
Father with osteoarthritis.
H. Social History
Non-smoker, occasional alcohol use, sedentary job.
II. Objective
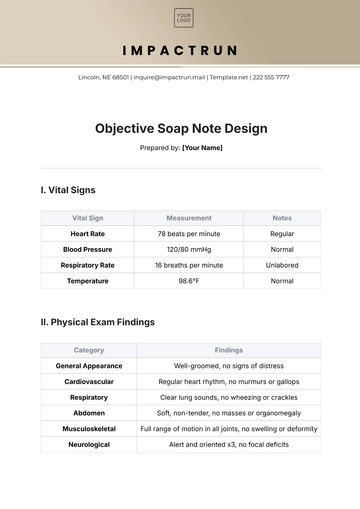
A. Vital Signs
Vital Sign | Measurement |
|---|---|
Temperature | 98.6°F |
Blood Pressure (BP) | 130/85 mmHg |
Heart Rate | 72 bpm |
Respiratory Rate | 16 bpm |
Weight | 180 lbs |
B. Physical Exam
Category | Findings |
|---|---|
General | Alert, no acute distress |
Musculoskeletal | Tenderness over the lumbar spine |
Neurological | Reflexes intact, no sensory deficits |
Range of Motion | Limited flexion due to pain |
III. Assessment
A. Primary Diagnosis
Mechanical lower back pain.
B. Differential Diagnosis
Lumbar strain or degenerative disc disease.
IV. Plan
A. Treatment
Recommend ibuprofen 400 mg every 6 hours as needed.
B. Follow-Up
Return in 2 weeks to assess progress.
C. Referrals
Physical therapy evaluation.
D. Patient Education
Advise posture correction and stretching exercises.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Elevate your clinical reporting with Template.net's Sample Soap Note Template. Designed for medical efficiency, this template is fully editable and customizable to suit diverse healthcare needs. Modify it seamlessly in our Ai Editor Tool, ensuring detailed, precise, and user-friendly patient documentation for all healthcare professionals.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note