Free Dehydration Case Study
I. Introduction
Dehydration is a common medical condition characterized by an inadequate fluid balance in the body, resulting in a depletion of bodily fluids. It can occur due to various factors such as excessive sweating, vomiting, diarrhea, or insufficient fluid intake. Understanding and effectively managing dehydration are crucial aspects of medical care, especially in vulnerable populations such as the elderly or those with chronic illnesses.
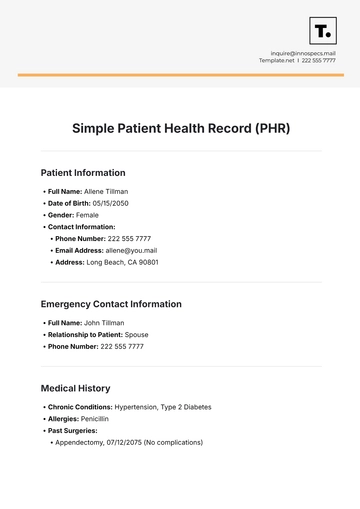
II . Patient Background
[Patient Name]
Age: [Age]
Gender: [Gender]
Occupation: [Occupation]
Medical History: Hypertension, Type 2 Diabetes
Presenting Complaint
Onset of symptoms: [Date]
Chief complaints: Fatigue, dry mouth, decreased urine output
Duration of symptoms: 2 days
III. Symptoms and Signs of Dehydration
3.1 Physical Examination Findings
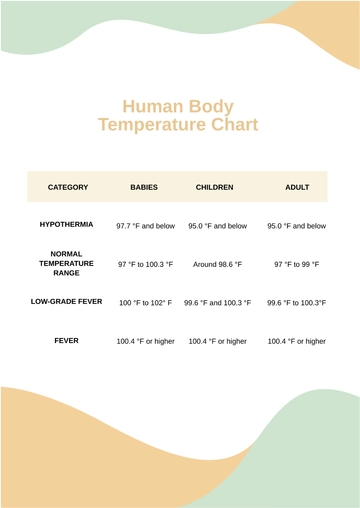
Vital signs: Blood Pressure (BP) of 110/70 mmHg indicates normal blood pressure for the patient. Heart Rate (HR) of 90 bpm is within the normal range for an adult at rest. A temperature of 98.6°F is within the normal range.
Skin turgor: Decreased skin turgor is a clinical sign of dehydration. Skin tenting noted on the forearm indicates delayed return of skin to its normal position after being pinched, which is indicative of reduced skin elasticity due to dehydration.
Mucous membranes: Dry mucous membranes, particularly the oral mucosa appearing sticky, suggest dehydration. Dryness and stickiness in the oral cavity are common manifestations of reduced body fluid levels.
3.2 Laboratory Investigations
Serum electrolytes: Sodium (Na) level of 135 mEq/L and Potassium (K) level of 3.5 mEq/L are within the normal range. However, slight deviations can still be significant in the context of dehydration.
Blood urea nitrogen (BUN) and creatinine: Blood urea nitrogen (BUN) levels of 25 mg/dL and creatinine levels of 1.2 mg/dL are within normal limits. These values help assess renal function and hydration status.
Urine specific gravity: A urine specific gravity of 1.030 indicates concentrated urine, which is a common finding in dehydrated individuals. It reflects the kidneys' ability to concentrate urine in response to decreased fluid intake.
Other relevant tests (CBC, CMP): Complete Blood Count (CBC) and Comprehensive Metabolic Panel (CMP) results are within normal limits, indicating no significant abnormalities in hematological parameters and organ function beyond what is expected in dehydration.
IV. Diagnostic Tests Conducted
4.1 Urinalysis
Purpose: The urinalysis is conducted to assess urine concentration and hydration status. It helps determine the kidney's ability to concentrate urine, which is crucial in evaluating dehydration.
Findings: The urinalysis showed an elevated urine specific gravity, indicating concentrated urine. This finding is suggestive of dehydration, as the body tries to conserve water by producing concentrated urine when fluid intake is insufficient.
4.2 Basic Metabolic Panel (BMP)
Purpose: The Basic Metabolic Panel (BMP) is performed to evaluate electrolyte levels and renal function. It includes tests such as sodium, potassium, and creatinine levels, which are essential in assessing hydration status and kidney function.
Findings: The BMP revealed mild hyponatremia (low sodium levels), which can occur in dehydration due to relative water excess compared to sodium levels. However, renal function, indicated by creatinine levels, was normal, suggesting adequate kidney function despite the electrolyte imbalance.
V. Treatment Administered
5.1 Fluid Replacement Therapy
Type of fluids: Intravenous normal saline (0.9% NaCl) solution, 1 liter, is administered to replenish lost fluids and correct dehydration. Normal saline is isotonic, closely resembling the body's natural fluid composition.
Route of administration: The fluid is administered intravenously to ensure rapid absorption and immediate correction of fluid and electrolyte imbalances.
Monitoring parameters: Hourly monitoring of fluid intake/output and vital signs (including blood pressure, heart rate, and temperature) is essential to track the patient's response to fluid therapy and detect any complications such as fluid overload or electrolyte disturbances.
5.2 Electrolyte Correction
Specific electrolytes targeted: Sodium levels are specifically targeted for correction, given the mild hyponatremia observed in the patient's lab results.
Medications administered: Oral sodium chloride tablets, 1 gram, are given to help increase sodium levels in the body. Sodium chloride tablets provide a controlled and measured dose of sodium.
Monitoring response: Serum electrolytes, including sodium levels, are monitored every 4 hours to assess the patient's response to electrolyte correction. Close monitoring helps prevent rapid fluctuations in electrolyte levels and ensures safe correction of hyponatremia.
VI. Outcomes of Treatment
6.1 Short-term Response
Improvement in symptoms: The patient experienced decreased fatigue and improved oral moisture following fluid replacement therapy and electrolyte correction. These improvements are indicative of the body's response to rehydration and electrolyte balance restoration.
Changes in laboratory parameters: There was an increase in serum sodium levels within the normal range, reflecting the successful correction of mild hyponatremia. Improved urine output suggests better renal function and hydration status.
6.2 Long-term Follow-up
Follow-up visits: Weekly follow-up visits are scheduled for the next month to monitor the patient's hydration status, electrolyte levels, and overall health. Regular monitoring helps prevent the recurrence of dehydration and electrolyte imbalances.
Maintenance therapy: The patient is prescribed oral rehydration solution (ORS) for home use to maintain adequate hydration levels. ORS helps replenish electrolytes and fluids lost through daily activities and prevents dehydration.
Patient education: The patient is taught about the necessity of proper hydration, especially in hot weather or during exercise. They're advised to watch for dehydration symptoms like intense thirst, dry mouth, or dark urine and get medical attention if they continue or worsen. This knowledge enables the patient to take steps to prevent dehydration.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Effortlessly analyze dehydration cases with Template.net's Case Study Template. Editable and customizable, this template streamlines data organization for thorough reporting and analysis. Utilize our Ai Editor Tool for easy customization and professional formatting, ensuring clear and concise case study presentations. Empower your team to communicate insights effectively, facilitating informed decisions and improved outcomes in managing dehydration cases.