Free Objective Soap Note Design
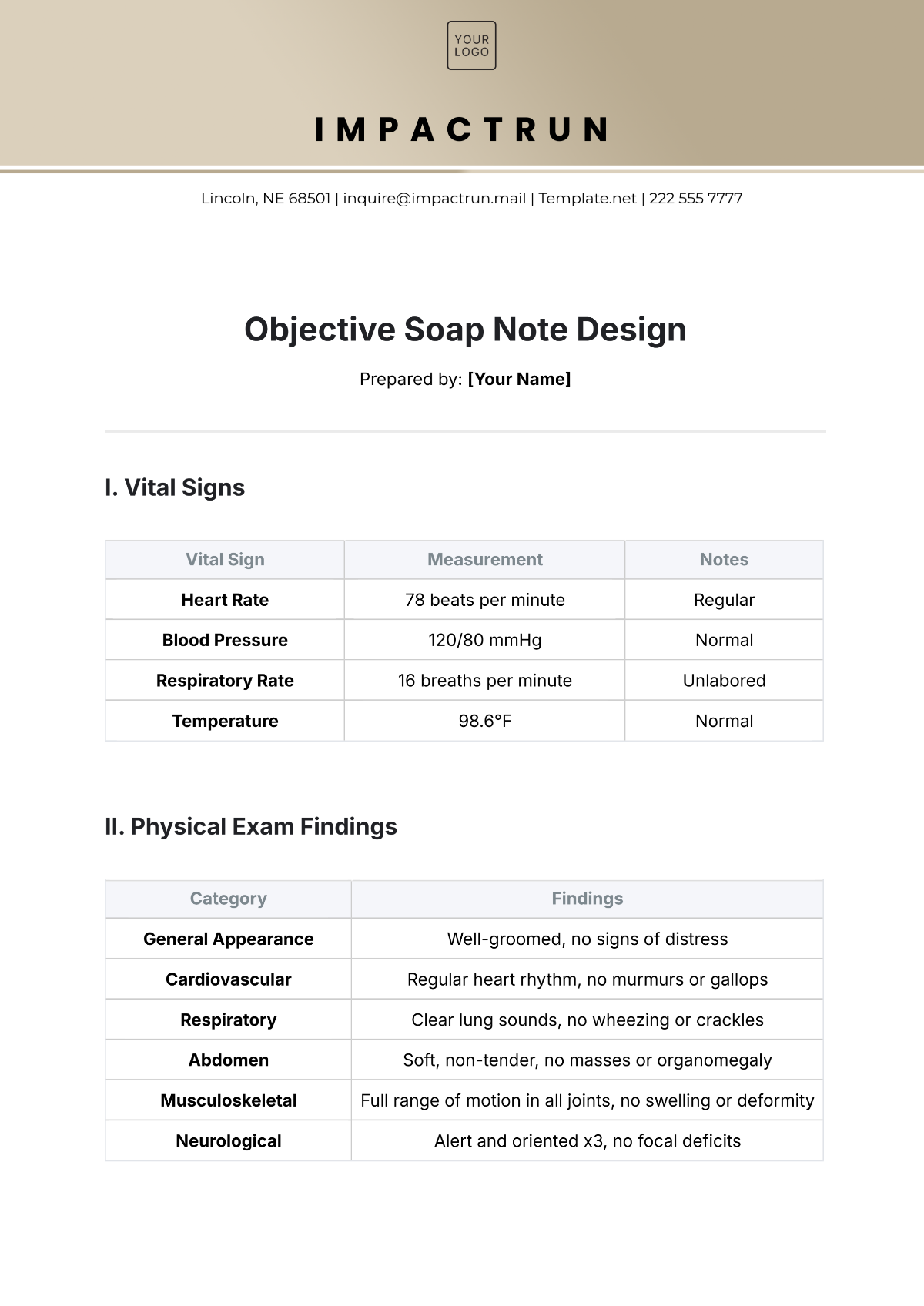
Prepared by: [Your Name]
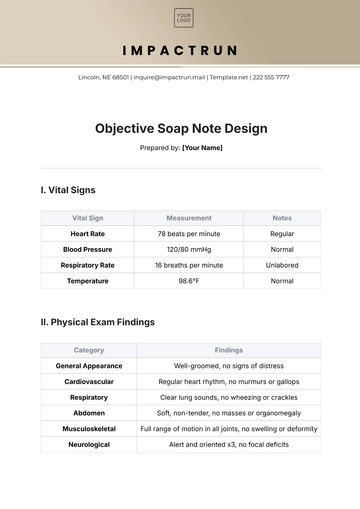
I. Vital Signs
Vital Sign | Measurement | Notes |
|---|---|---|
Heart Rate | 78 beats per minute | Regular |
Blood Pressure | 120/80 mmHg | Normal |
Respiratory Rate | 16 breaths per minute | Unlabored |
Temperature | 98.6°F | Normal |
II. Physical Exam Findings
Category | Findings |
|---|---|
General Appearance | Well-groomed, no signs of distress |
Cardiovascular | Regular heart rhythm, no murmurs or gallops |
Respiratory | Clear lung sounds, no wheezing or crackles |
Abdomen | Soft, non-tender, no masses or organomegaly |
Musculoskeletal | Full range of motion in all joints, no swelling or deformity |
Neurological | Alert and oriented x3, no focal deficits |
III. Laboratory Results
Test | Result | Normal Range |
|---|---|---|
Complete Blood Count (CBC) | ||
Hemoglobin | 14 g/dL | 12–16 g/dL (female), 14–18 g/dL (male) |
White Blood Cell Count | 6,000/mm³ | 4,000–11,000/mm³ |
Platelets | 250,000/mm³ | 150,000–450,000/mm³ |
Test | Result | Normal Range |
|---|---|---|
Basic Metabolic Panel (BMP) | ||
Sodium | 140 mEq/L | 135–145 mEq/L |
Potassium | 4.2 mEq/L | 3.5–5.0 mEq/L |
Creatinine | 1.0 mg/dL | 0.6–1.2 mg/dL |
Glucose | 90 mg/dL | 70–100 mg/dL (fasting) |
Test | Result | Normal Range |
|---|---|---|
Liver Function Tests | ||
AST (Aspartate Aminotransferase) | 22 U/L | 10–40 U/L |
ALT (Alanine Aminotransferase) | 24 U/L | 7–56 U/L |
Bilirubin | 0.8 mg/dL | 0.1–1.2 mg/dL |
IV. Diagnostic Tests
Chest X-ray: No acute pulmonary disease, clear lung fields
Electrocardiogram (EKG): Normal sinus rhythm, no ST elevation or depression
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Document with precision using our Objective SOAP Note Design Template, available at Template.net. This template emphasizes clear and concise recording of objective medical findings. It is fully editable and customizable, allowing you to tailor it to your unique documentation needs. Easily personalize this design editable in our AI Editor Tool, ensuring efficiency and accuracy in your workflow.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
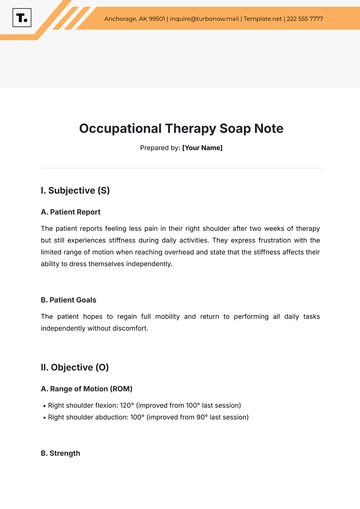
- SOAP Note Templates
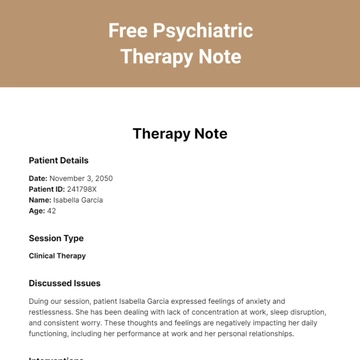
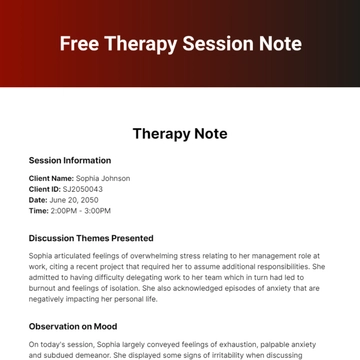
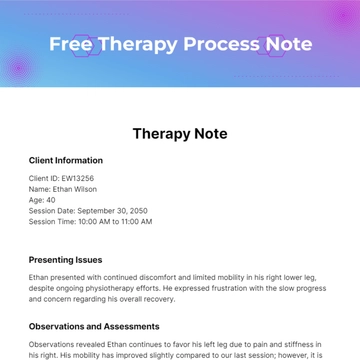
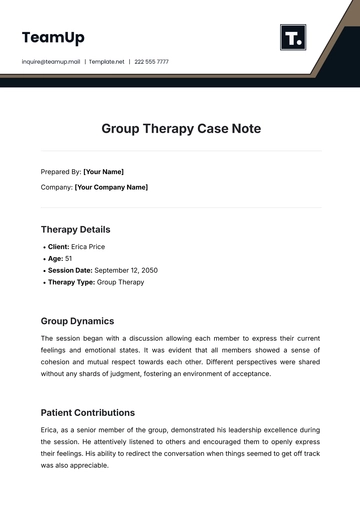
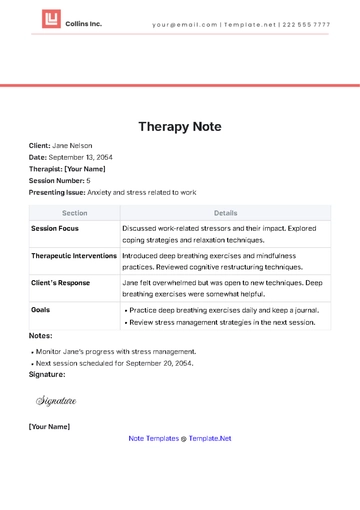
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note