Free Nursing Home Assessment Documentation
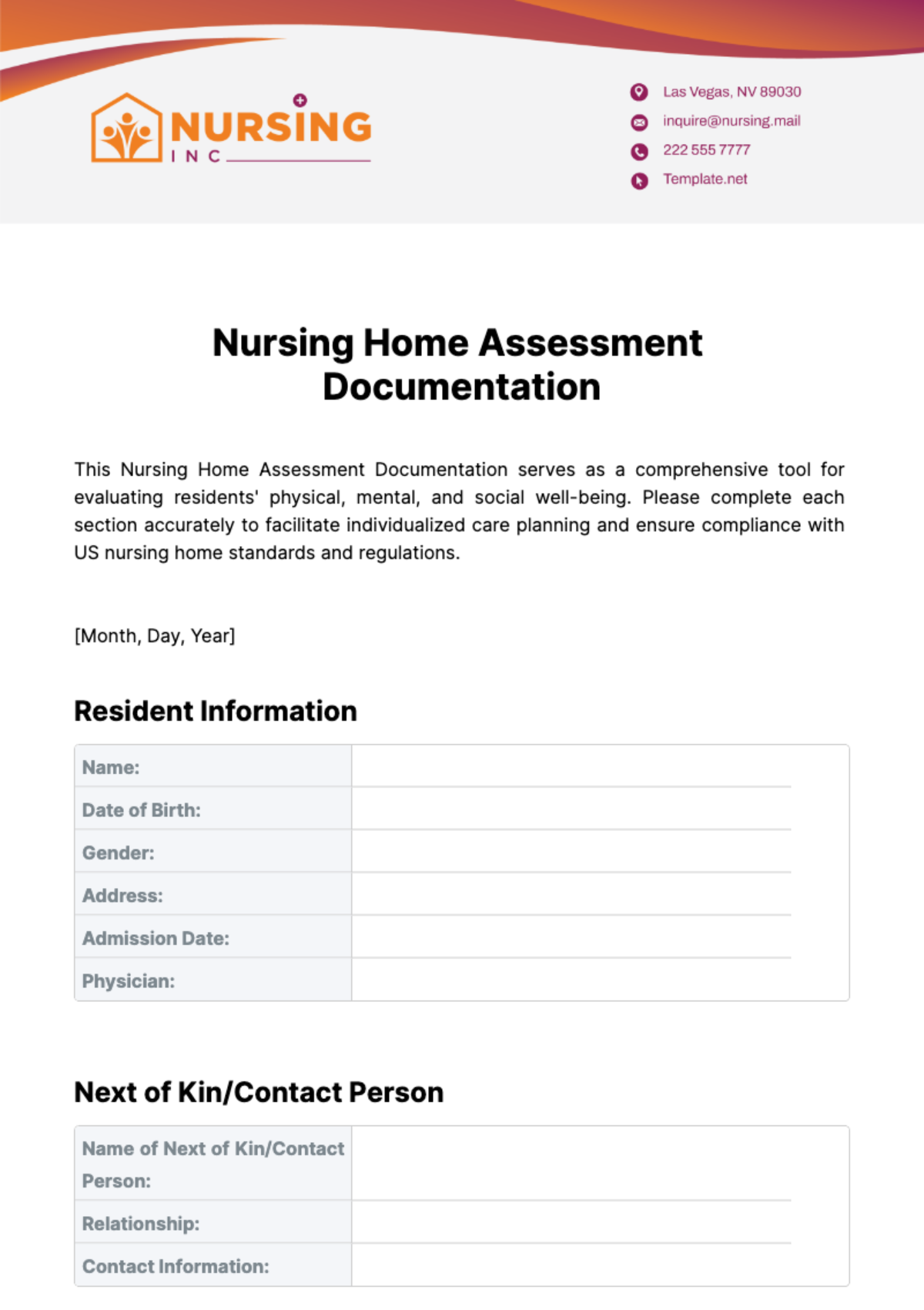
This Nursing Home Assessment Documentation serves as a comprehensive tool for evaluating residents' physical, mental, and social well-being. Please complete each section accurately to facilitate individualized care planning and ensure compliance with US nursing home standards and regulations.
[Month, Day, Year]
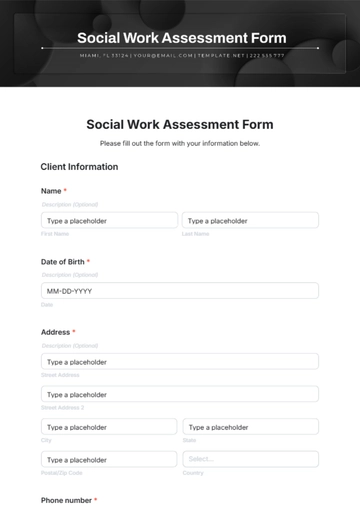
Resident Information
Name: | |
|---|---|
Date of Birth: | |
Gender: | |
Address: | |
Admission Date: | |
Physician: |
Next of Kin/Contact Person
Name of Next of Kin/Contact Person: | |
|---|---|
Relationship: | |
Contact Information: |
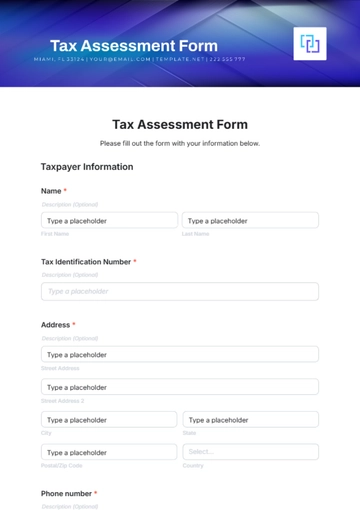
Assessment Details
Physical Health Assessment | |
Vital Signs: | Blood Pressure: Heart Rate: Respiratory Rate: Temperature: |
Mobility Status: | |
Skin Integrity: | |
Nutrition Status: | |
Activities of Daily Living (ADLs): | |
Mental Health Assessment | |
Cognitive Function: | |
Mood and Affect: | |
Behavioral Observations: | |
Medication Management | |
Current Medications: | |
Allergies: | |
Social and Emotional Assessment | |
Social Support System: | |
Emotional Well-being: | |
Safety Assessment | |
Fall Risk: | |
Environmental Safety: | |
Emergency Preparedness: | |
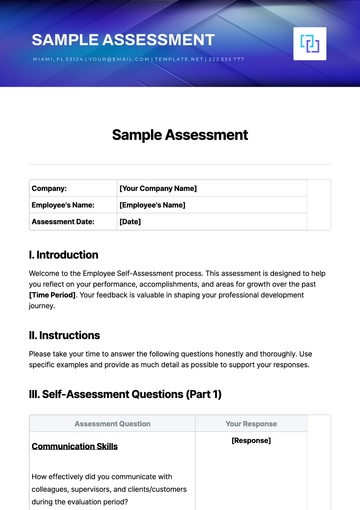
Care Plan
Based on the assessment findings, the following care plan is recommended:
Follow-Up Plan
Regular Follow-Up Assessments: | |
Consultations with Specialists: | |
Family Meetings: |
Signature Section

[Month, Day, Year]

[Month, Day, Year]
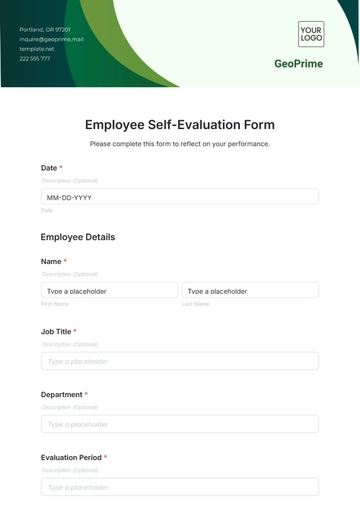
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline resident evaluations with the Nursing Home Assessment Documentation Template from Template.net. This editable and customizable template facilitates thorough assessments of residents' needs and conditions, aiding in personalized care planning. Editable in our Ai Editor Tool, it's crucial for ensuring accurate, comprehensive documentation, supporting optimal care delivery, and enhancing resident well-being in your nursing home.