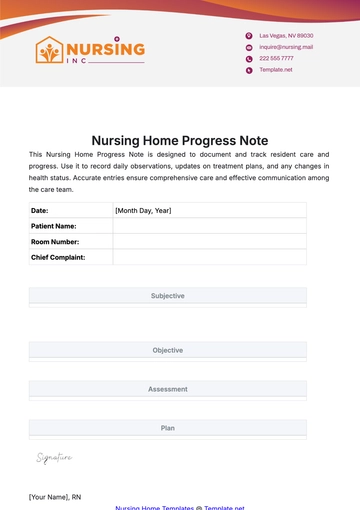
Free Nursing Home Discharge Summary
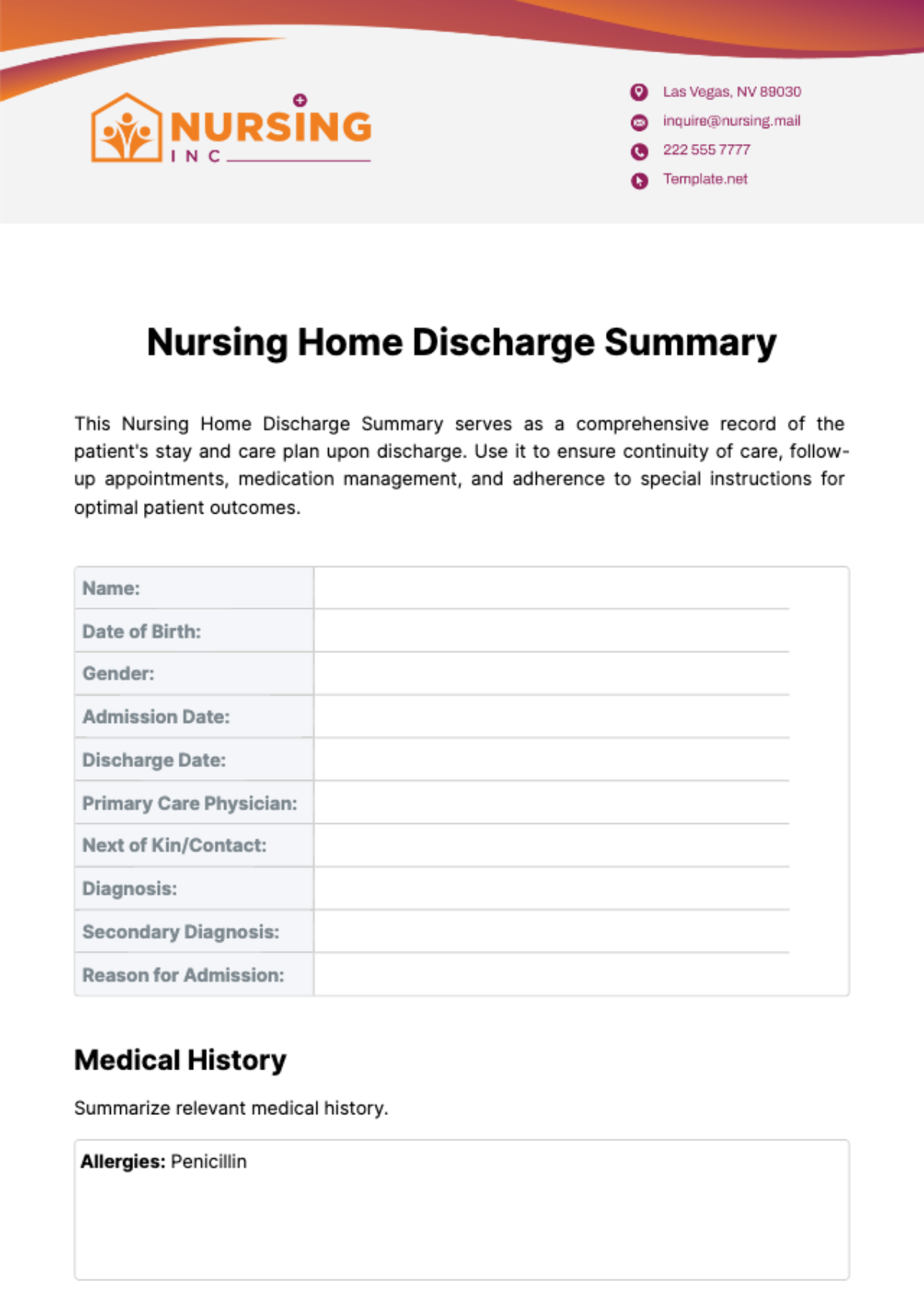
This Nursing Home Discharge Summary serves as a comprehensive record of the patient's stay and care plan upon discharge. Use it to ensure continuity of care, follow-up appointments, medication management, and adherence to special instructions for optimal patient outcomes.
Name: | |
|---|---|
Date of Birth: | |
Gender: | |
Admission Date: | |
Discharge Date: | |
Primary Care Physician: | |
Next of Kin/Contact: | |
Diagnosis: | |
Secondary Diagnosis: | |
Reason for Admission: |
Medical History
Summarize relevant medical history.
Allergies: Penicillin |
Treatment and Care Received
Describe any treatment and care received (include frequency and focus areas).
Physical Therapy: Daily sessions focusing on mobility and strength |
Functional Status
Describe the mobility status, level of assistance needed, feeding abilities, and continence status.
ADLs (Activities of Daily Living) | |
Mobility: | Requires walker, able to walk short distances with assistance |
Hygiene: | Needs assistance with bathing and dressing |
Feeding: | Independent, uses adaptive utensils |
Continence: | Incontinent, uses adult diapers |
Cognitive Status
Describe the cognitive status, including orientation and memory.
Oriented to person and place, occasional memory lapses |
Discharge Plan
List all medications and details of any follow-up appointments.
Medications: | Amlodipine 10 mg daily |
Follow-up Appointments: | Primary Care Physician: [Month, Day, Year] |
Home Health Care Services: | Visiting Nurse: Twice weekly for wound care and medication management |
Special Instructions: | Low-sodium diet |
Recommendations/Considerations
List any recommendations or considerations for ongoing care, such as monitoring for signs of infection.
Monitor for signs of infection at the surgical site |
Comments/Notes
Add any additional comments or notes for progress and discharge plan.
Patient has shown significant improvement in mobility and speech |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Coordinate care transitions smoothly with the Nursing Home Discharge Summary Template from Template.net. This editable and customizable template ensures comprehensive documentation of a resident's care journey, treatments, and recommendations upon discharge. Editable in our Ai Editor Tool, it's essential for facilitating clear communication between healthcare providers, residents, and their families, ensuring continuity of care and supporting successful transitions from your nursing home.