Free Professional Nursing Assessment Checklist
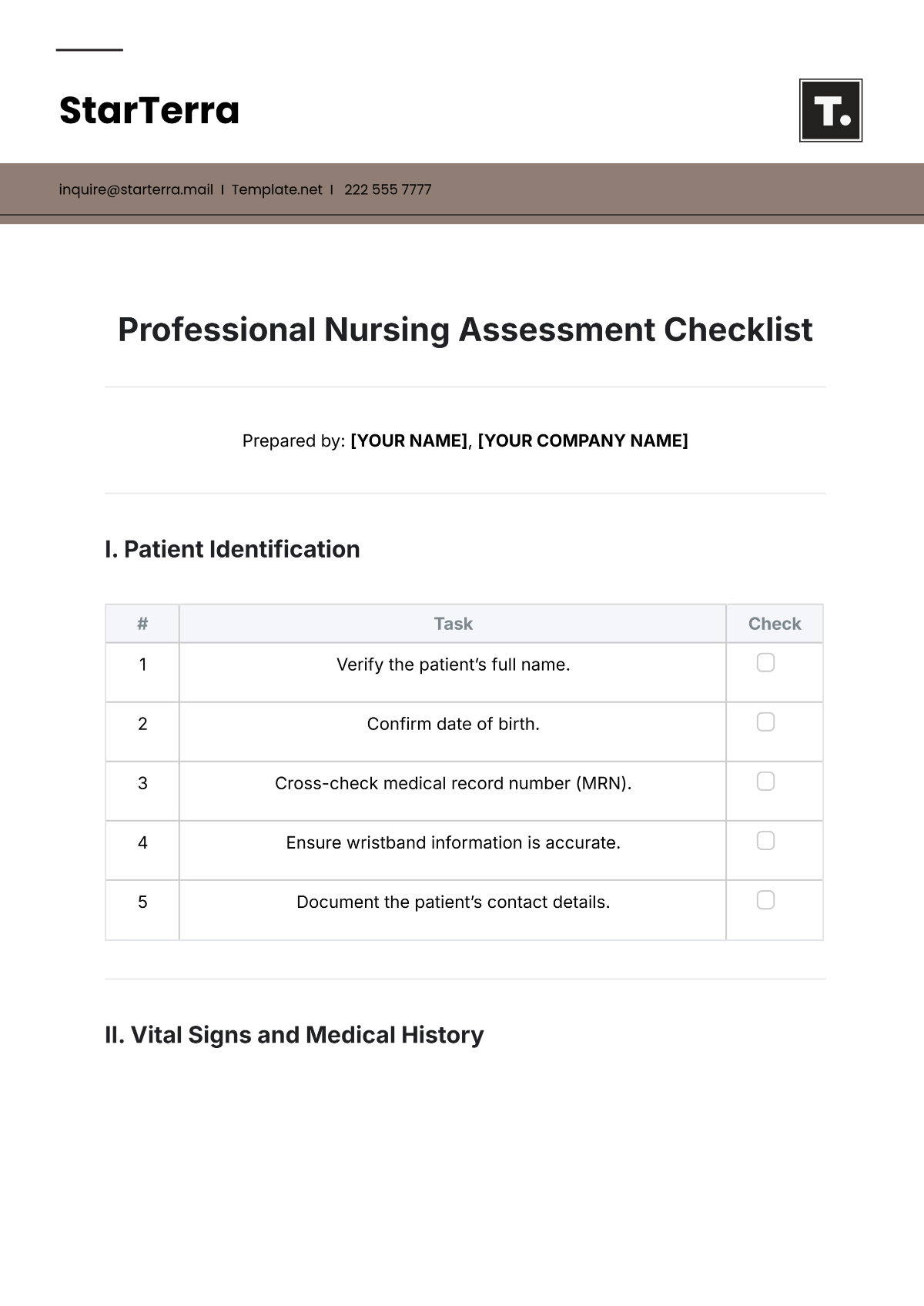
Prepared by: [YOUR NAME], [YOUR COMPANY NAME]
I. Patient Identification
# | Task | Check |
|---|---|---|
1 | Verify the patient’s full name. | |
2 | Confirm date of birth. | |
3 | Cross-check medical record number (MRN). | |
4 | Ensure wristband information is accurate. | |
5 | Document the patient’s contact details. |
II. Vital Signs and Medical History
# | Task | Check |
|---|---|---|
1 | Measure and record body temperature. | |
2 | Take pulse rate, respiratory rate, and blood pressure. | |
3 | Monitor oxygen saturation levels (SpO2). | |
4 | Review chronic conditions and current medications. | |
5 | Note any allergies and surgical history. |
III. Physical Examination
# | Task | Check |
|---|---|---|
1 | Inspect the skin for wounds, rashes, or discoloration. | |
2 | Assess mobility and range of motion. | |
3 | Check the respiratory system (e.g., lung sounds). | |
4 | Evaluate the cardiovascular system (e.g., heart sounds, circulation). | |
5 | Palpate the abdomen for tenderness or abnormalities. |
IV. Pain and Mental Health Assessment
# | Task | Check |
|---|---|---|
1 | Determine pain level using a scale (0–10). | |
2 | Identify pain location, duration, and nature. | |
3 | Observe emotional state (e.g., calm, agitated). | |
4 | Assess cognitive function and behavioral patterns. | |
5 | Screen for signs of anxiety or depression. |
V. Nutritional and Hydration Status
# | Task | Check |
|---|---|---|
1 | Review dietary intake and feeding habits. | |
2 | Check hydration levels (fluid intake/output). | |
3 | Assess for signs of malnutrition or obesity. | |
4 | Identify any dietary restrictions. | |
5 | Recommend nutritional interventions if needed. |
VI. Nursing Diagnoses and Care Plan
# | Task | Check |
|---|---|---|
1 | Summarize findings from the assessment. | |
2 | Identify key nursing diagnoses. | |
3 | Develop a care plan based on the findings. | |
4 | Communicate care plans with the healthcare team. | |
5 | Educate the patient and family about the care plan. |
VII. Documentation and Finalization
# | Task | Check |
|---|---|---|
1 | Review the completed checklist for accuracy. | |
2 | Sign and date the completed assessment. | |
3 | File the checklist in the patient’s medical record. | |
4 | Update the electronic health record (EHR) if applicable. | |
5 | Confirm checklist completion with a supervisor if required. |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Uplift healthcare standards with our Nursing Assessment Checklist Template, available exclusively on Template.net. This highly editable and customizable tool streamlines nursing assessments for optimal patient care. Harness the power of our AI Editor Tool to effortlessly customize this checklist, ensuring precise and personalized assessments aligned with the highest healthcare standards.
You may also like
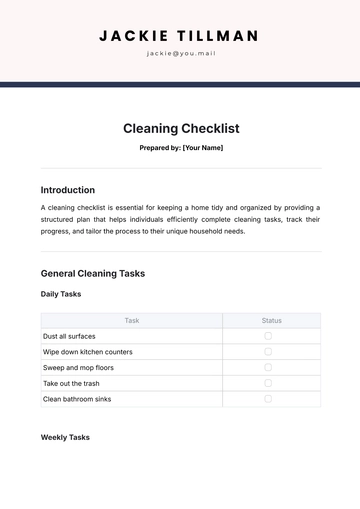
- Cleaning Checklist
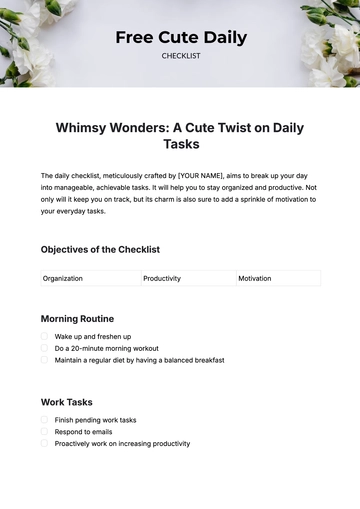
- Daily Checklist
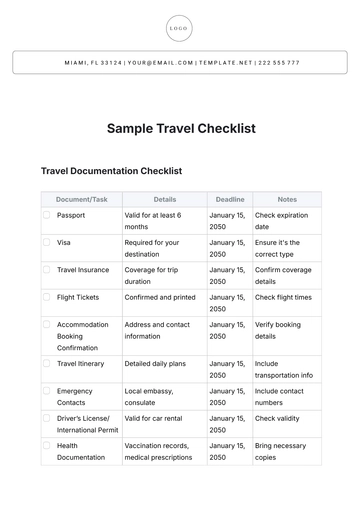
- Travel Checklist
- Self Care Checklist
- Risk Assessment Checklist
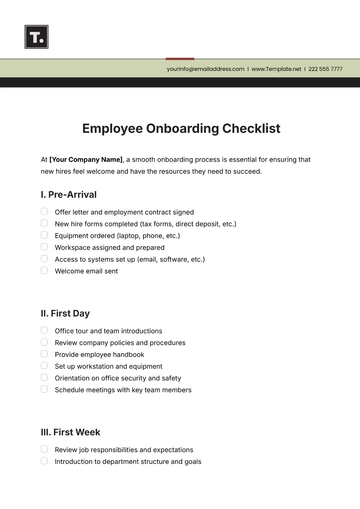
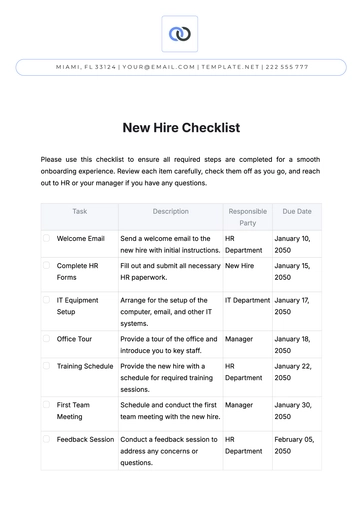
- Onboarding Checklist
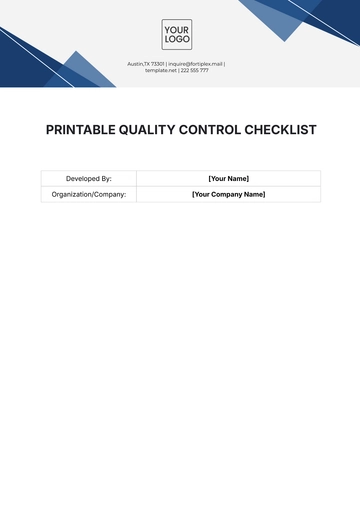
- Quality Checklist
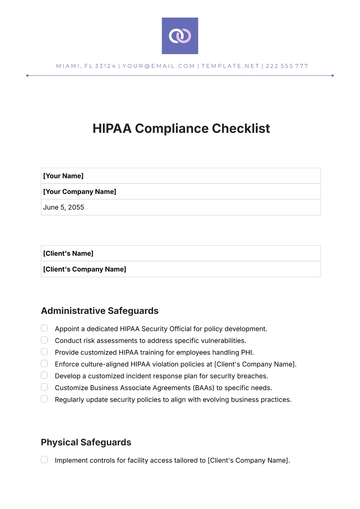
- Compliance Checklist
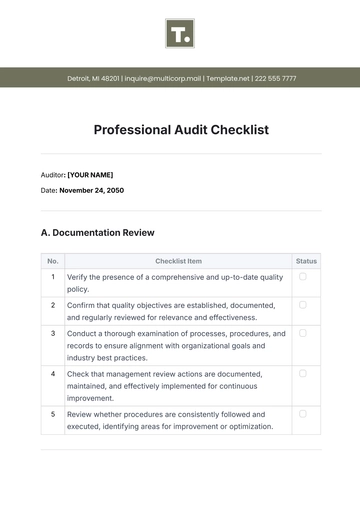
- Audit Checklist
- Registry Checklist
- HR Checklist
- Restaurant Checklist
- Checklist Layout
- Creative Checklist
- Sales Checklist
- Construction Checklist
- Task Checklist
- Professional Checklist
- Hotel Checklist
- Employee Checklist
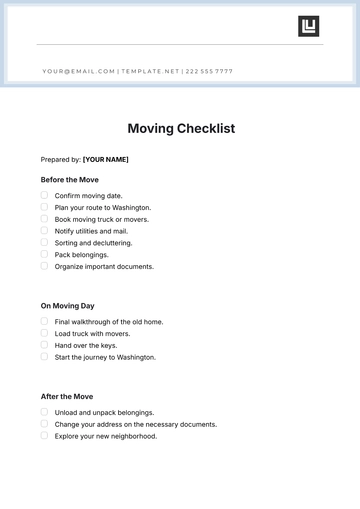
- Moving Checklist
- Marketing Checklist
- Accounting Checklist
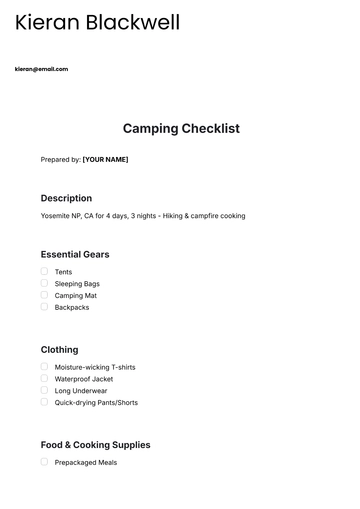
- Camping Checklist
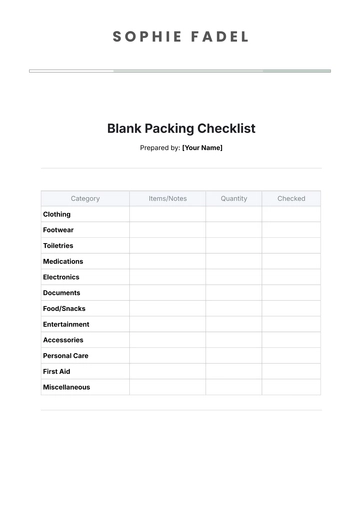
- Packing Checklist
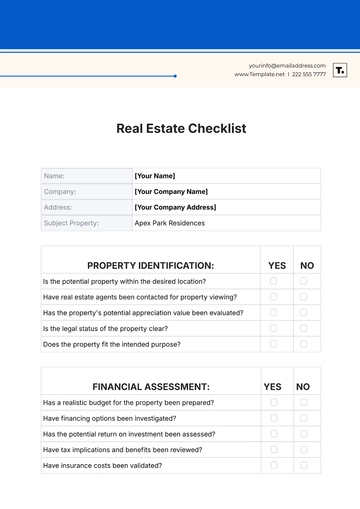
- Real Estate Checklist
- Cleaning Checklist Service
- New Employee Checklist
- Food Checklist
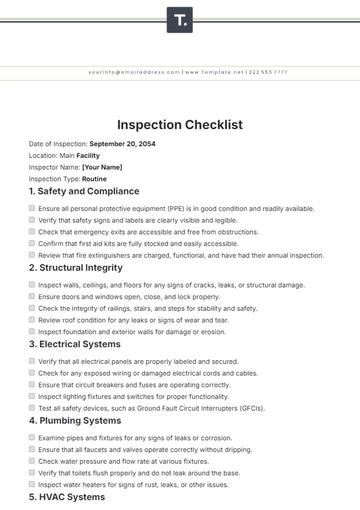
- Home Inspection Checklist
- Advertising Checklist
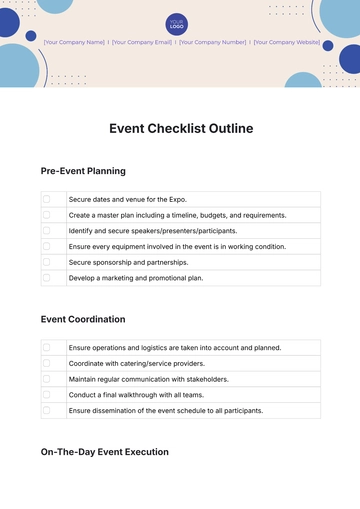
- Event Checklist
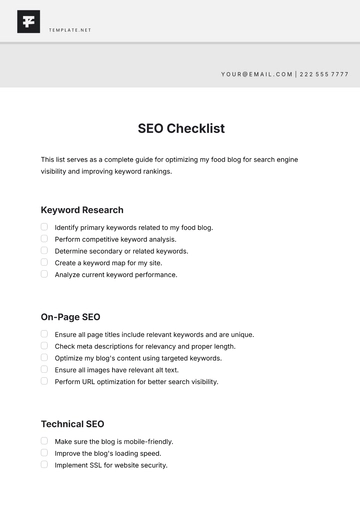
- SEO Checklist
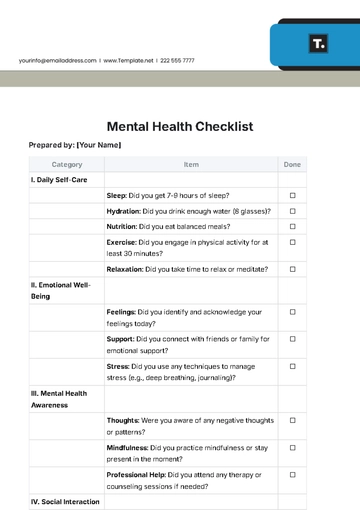
- Assessment Checklist
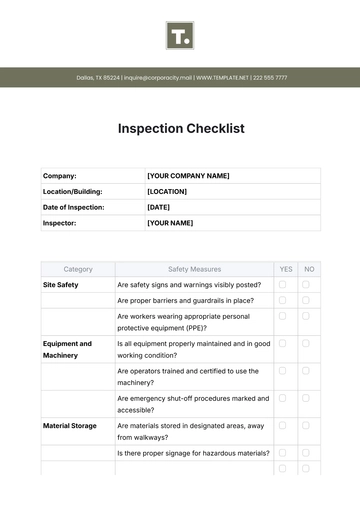
- Inspection Checklist
- Baby Registry Checklist
- Induction Checklist
- Employee Training Checklist
- Medical Checklist
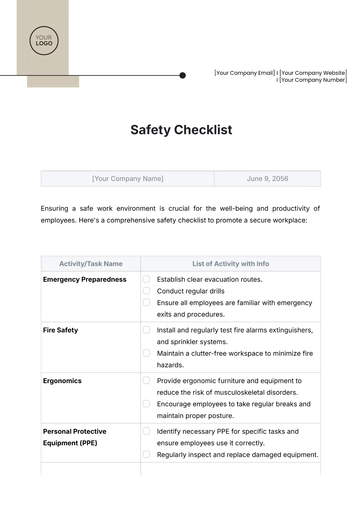
- Safety Checklist
- Site Checklist
- Job Checklist
- Service Checklist
- Nanny Checklist
- Building Checklist
- Work Checklist
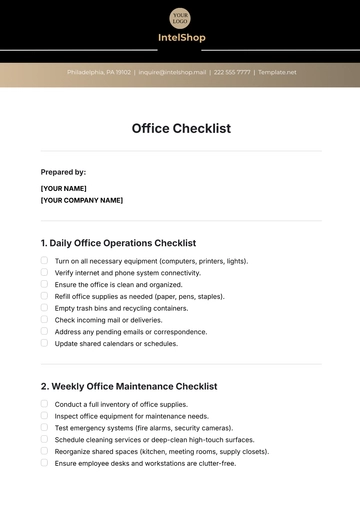
- Office Checklist
- Training Checklist
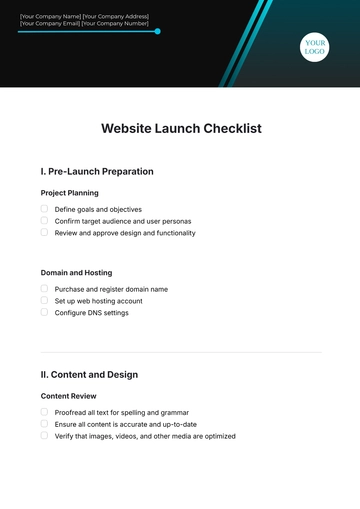
- Website Checklist
- IT and Software Checklist
- Performance Checklist
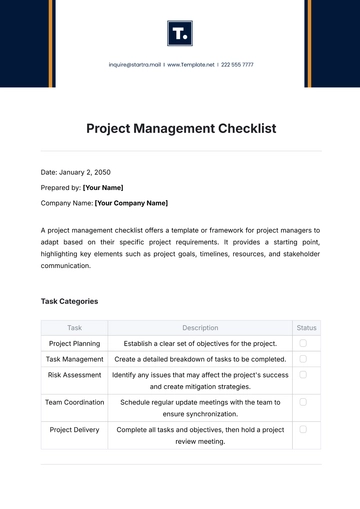
- Project Checklist
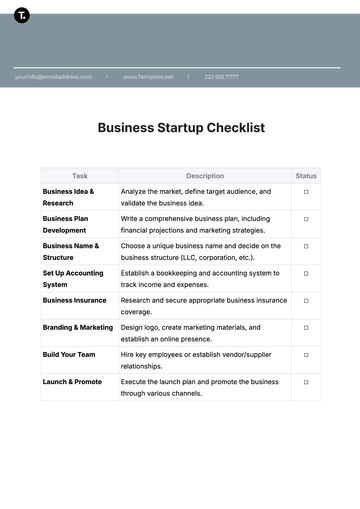
- Startup Checklist
- Education Checklist
- Home Checklist
- School Checklist
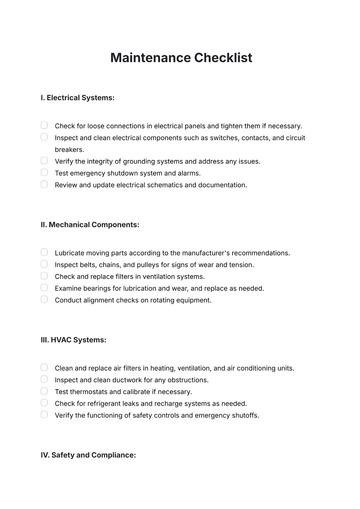
- Maintenance Checklist
- Planning Checklist
- Manager Checklist
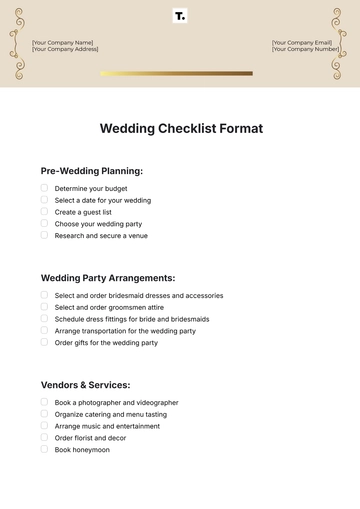
- Wedding Checklist
- Vehicle Checklist
- Travel Agency Checklist
- Vehicle Inspection Checklist
- Interior Design Checklist
- Backpacking Checklist
- Business Checklist
- Legal Checklist
- Nursing Home Checklist
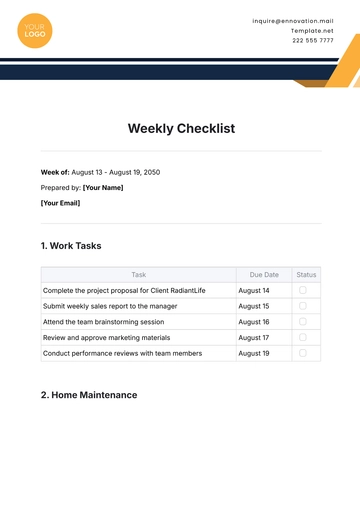
- Weekly Checklist
- Recruitment Checklist
- Salon Checklist
- Baby Checklist
- Equipment Checklist
- Trade Show Checklist
- Party Checklist
- Hospital Bag Checklist
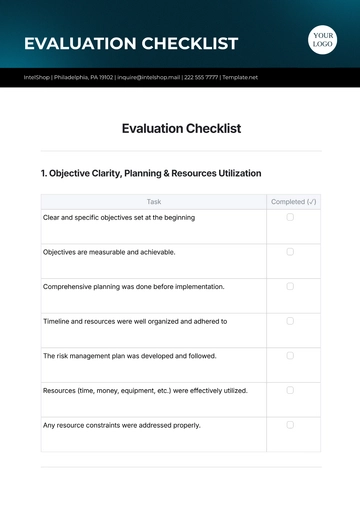
- Evaluation Checklist
- Agency Checklist
- First Apartment Checklist
- Hiring Checklist
- Opening Checklist
- Small Business Checklist
- Rental Checklist
- College Dorm Checklist
- New Puppy Checklist
- University Checklist
- Building Maintenance Checklist
- Work From Home Checklist
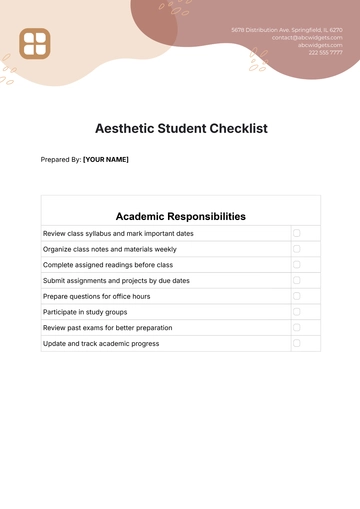
- Student Checklist
- Application Checklist