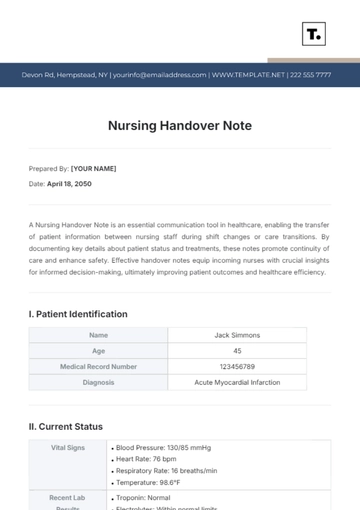
Free SBAR Nursing Notes
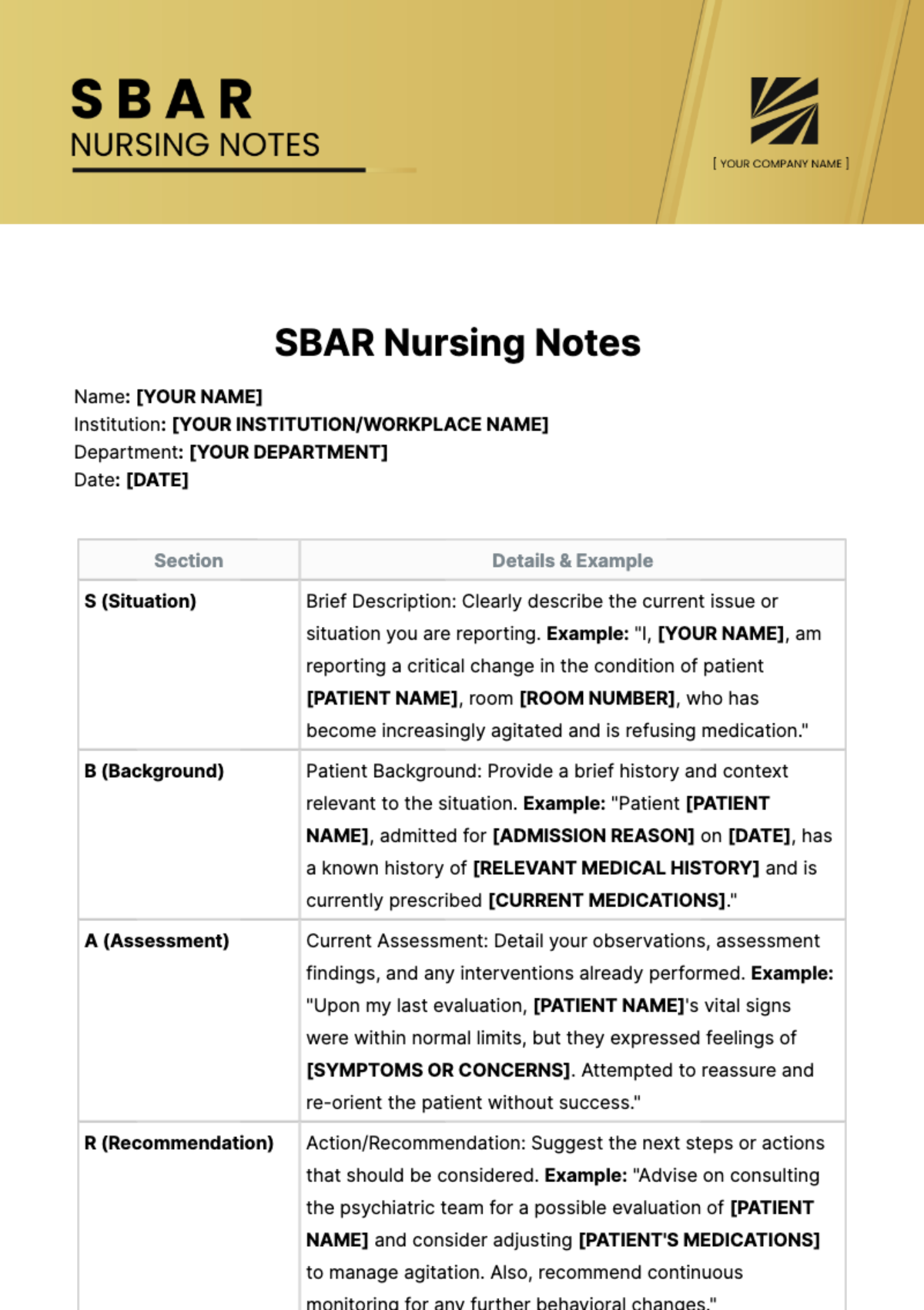
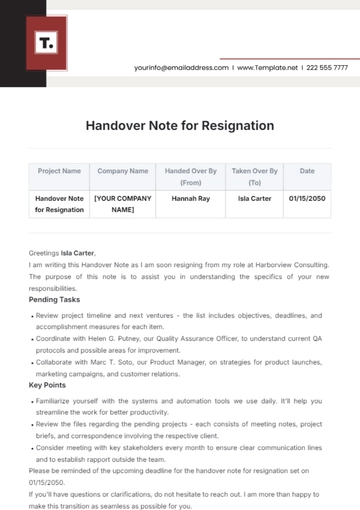
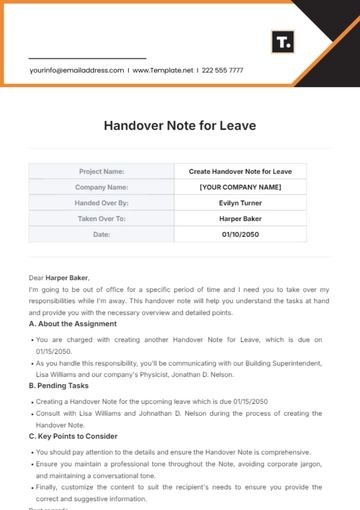
Name: [YOUR NAME]
Institution: [YOUR INSTITUTION/WORKPLACE NAME]
Department: [YOUR DEPARTMENT]
Date: [DATE]
Section | Details & Example |
|---|---|
S (Situation) | Brief Description: Clearly describe the current issue or situation you are reporting. Example: "I, [YOUR NAME], am reporting a critical change in the condition of patient [PATIENT NAME], room [ROOM NUMBER], who has become increasingly agitated and is refusing medication." |
B (Background) | Patient Background: Provide a brief history and context relevant to the situation. Example: "Patient [PATIENT NAME], admitted for [ADMISSION REASON] on [DATE], has a known history of [RELEVANT MEDICAL HISTORY] and is currently prescribed [CURRENT MEDICATIONS]." |
A (Assessment) | Current Assessment: Detail your observations, assessment findings, and any interventions already performed. Example: "Upon my last evaluation, [PATIENT NAME]'s vital signs were within normal limits, but they expressed feelings of [SYMPTOMS OR CONCERNS]. Attempted to reassure and re-orient the patient without success." |
R (Recommendation) | Action/Recommendation: Suggest the next steps or actions that should be considered. Example: "Advise on consulting the psychiatric team for a possible evaluation of [PATIENT NAME] and consider adjusting [PATIENT'S MEDICATIONS] to manage agitation. Also, recommend continuous monitoring for any further behavioral changes." |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Revamp your nursing notes with our SBAR Nursing Notes Template. Discover a suite of editable and customizable document templates tailored to streamline your workflow. Unlock efficiency with our Ai Editor Tool. Elevate your documentation process today with Template.net.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
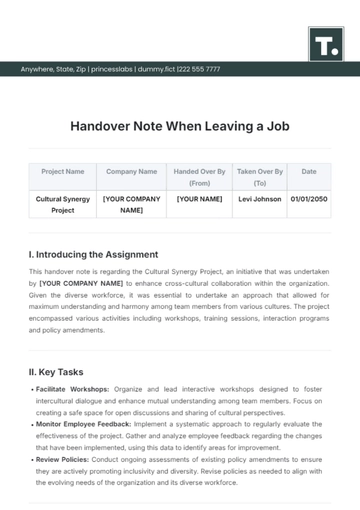
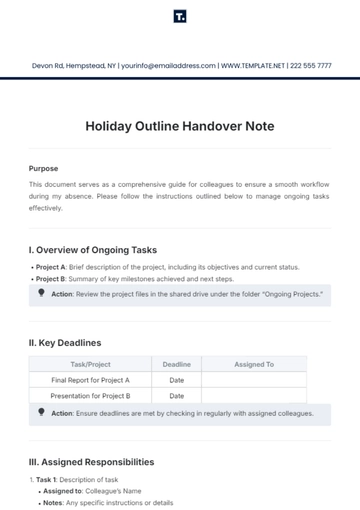
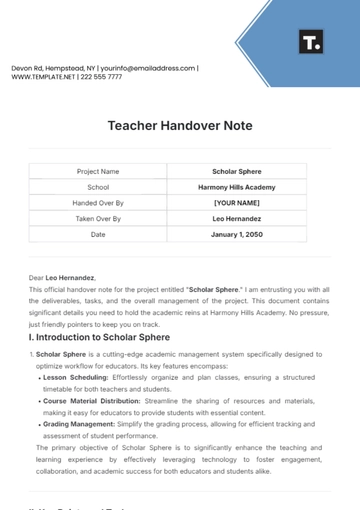
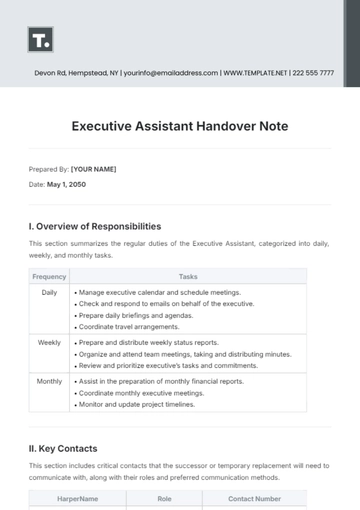
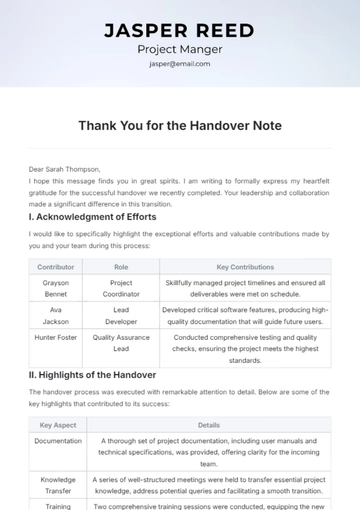
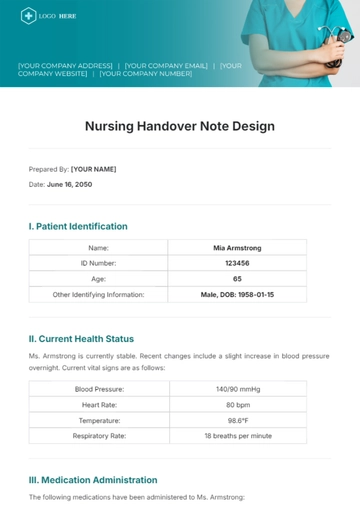
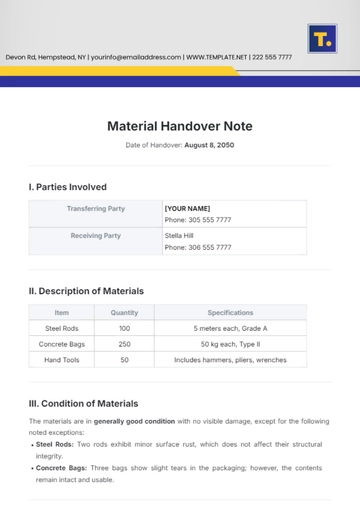
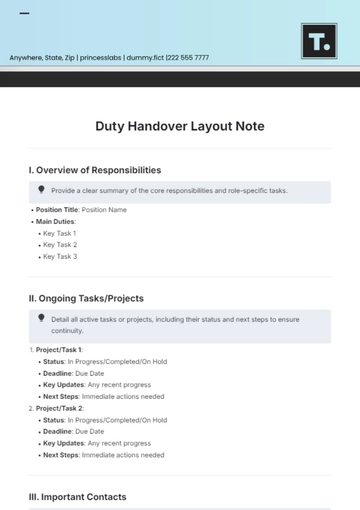
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note