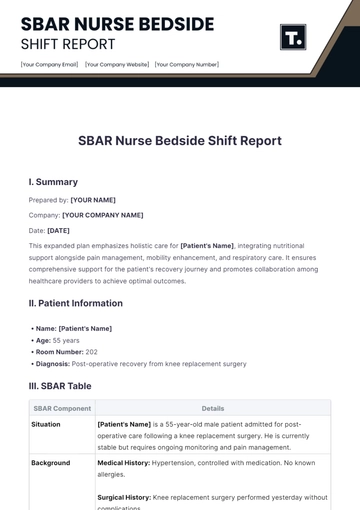
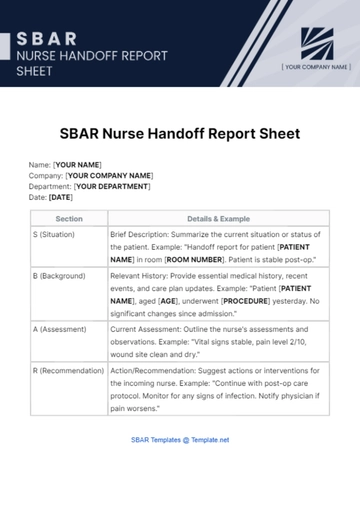
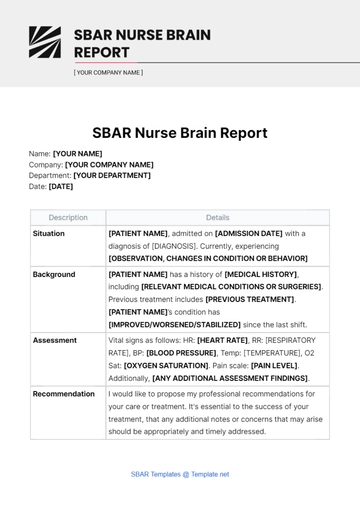
Free SBAR Nurse Handoff Report Sheet
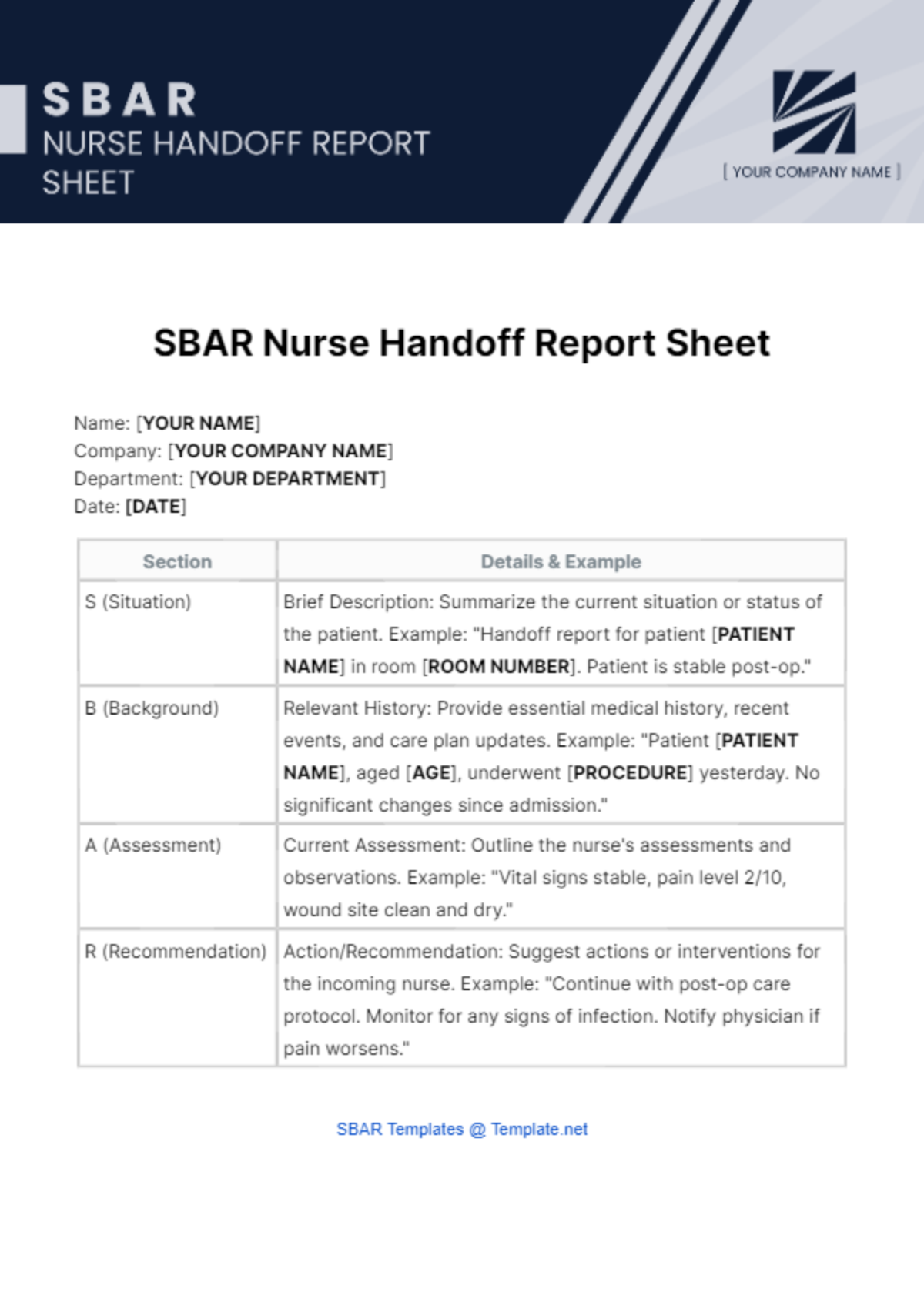
Name: [YOUR NAME]
Company: [YOUR COMPANY NAME]
Department: [YOUR DEPARTMENT]
Date: [DATE]
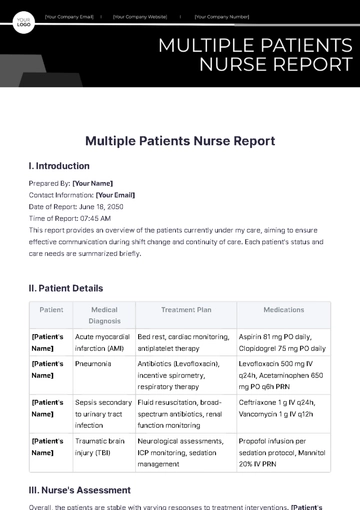
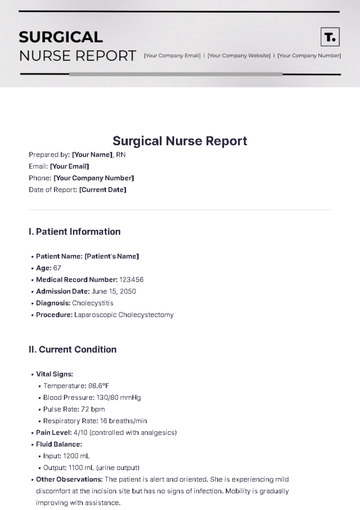
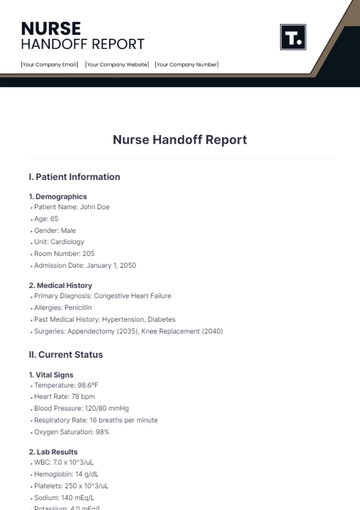
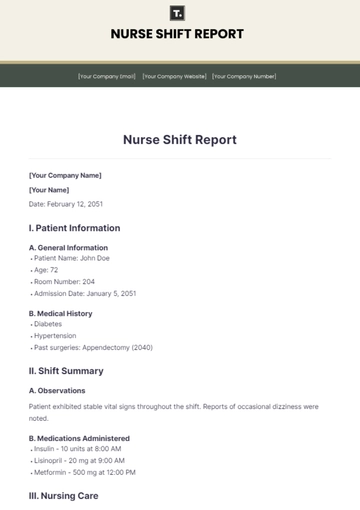
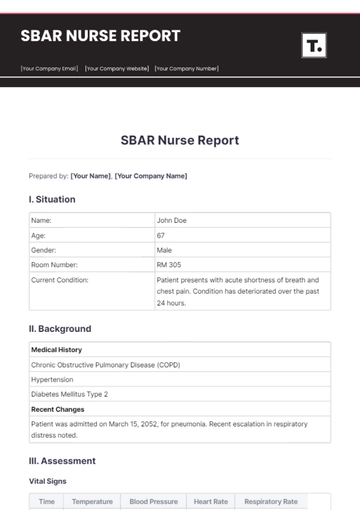
Section | Details & Example |
|---|---|
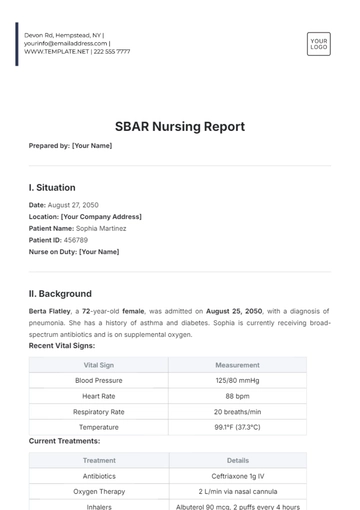
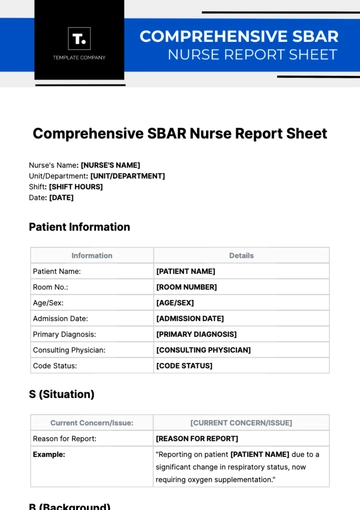
S (Situation) | Brief Description: Summarize the current situation or status of the patient. Example: "Handoff report for patient [PATIENT NAME] in room [ROOM NUMBER]. Patient is stable post-op." |
B (Background) | Relevant History: Provide essential medical history, recent events, and care plan updates. Example: "Patient [PATIENT NAME], aged [AGE], underwent [PROCEDURE] yesterday. No significant changes since admission." |
A (Assessment) | Current Assessment: Outline the nurse's assessments and observations. Example: "Vital signs stable, pain level 2/10, wound site clean and dry." |
R (Recommendation) | Action/Recommendation: Suggest actions or interventions for the incoming nurse. Example: "Continue with post-op care protocol. Monitor for any signs of infection. Notify physician if pain worsens." |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the SBAR Nurse Handoff Report Sheet Template from Template.net! This editable and customizable tool streamlines communication during shift transitions. Crafted for efficiency, it's editable in our Ai Editor Tool, ensuring seamless adaptation to your facility's needs. Elevate patient care with clarity and precision.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
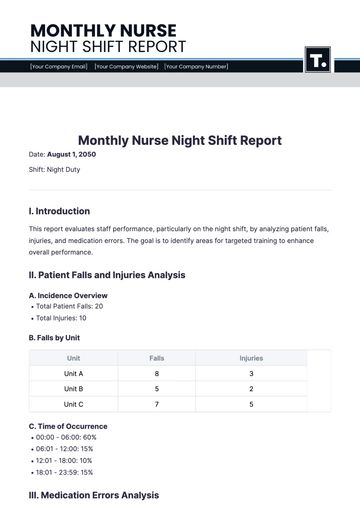
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
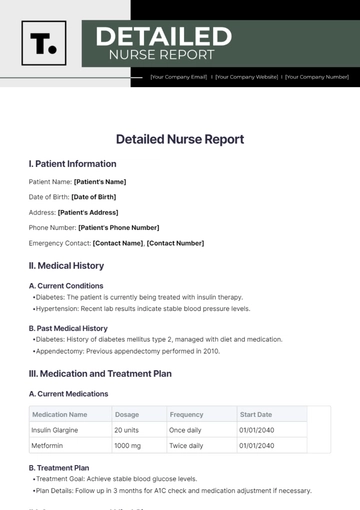
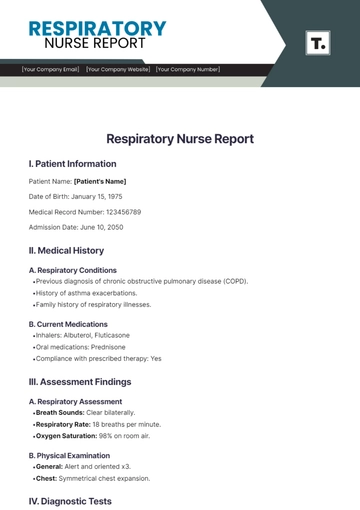
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
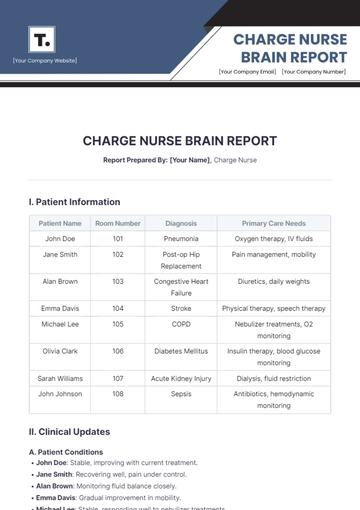
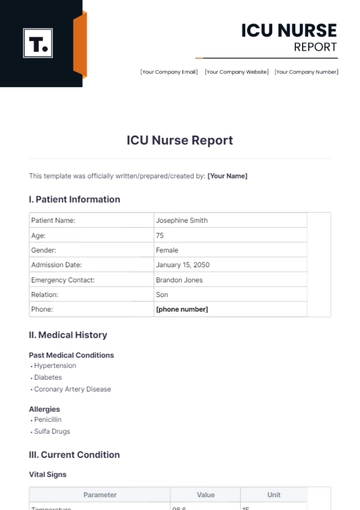
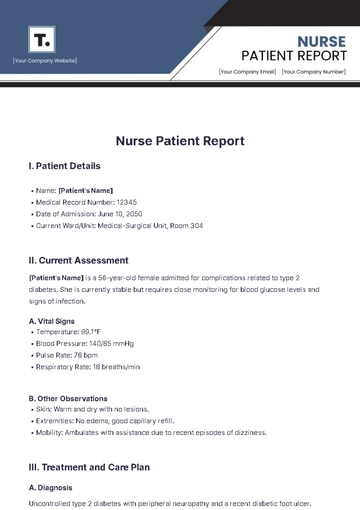
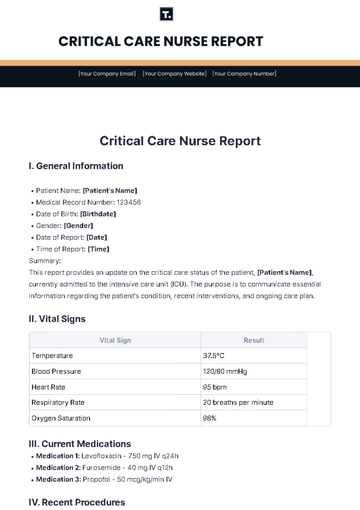
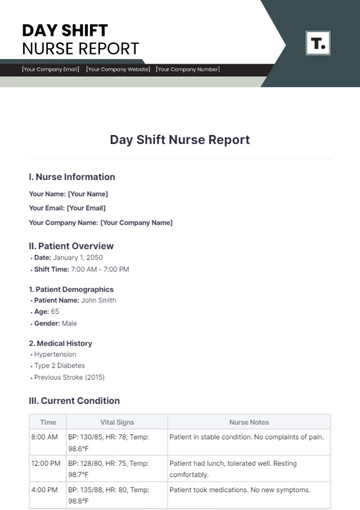
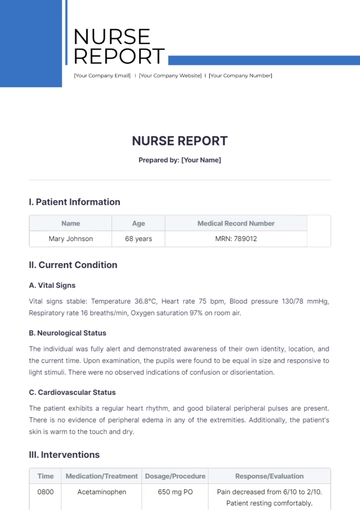
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report