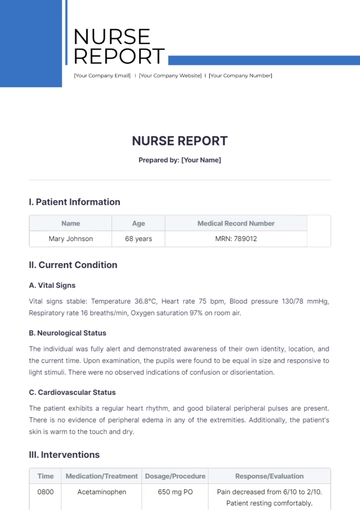
Free Nurse Patient Report
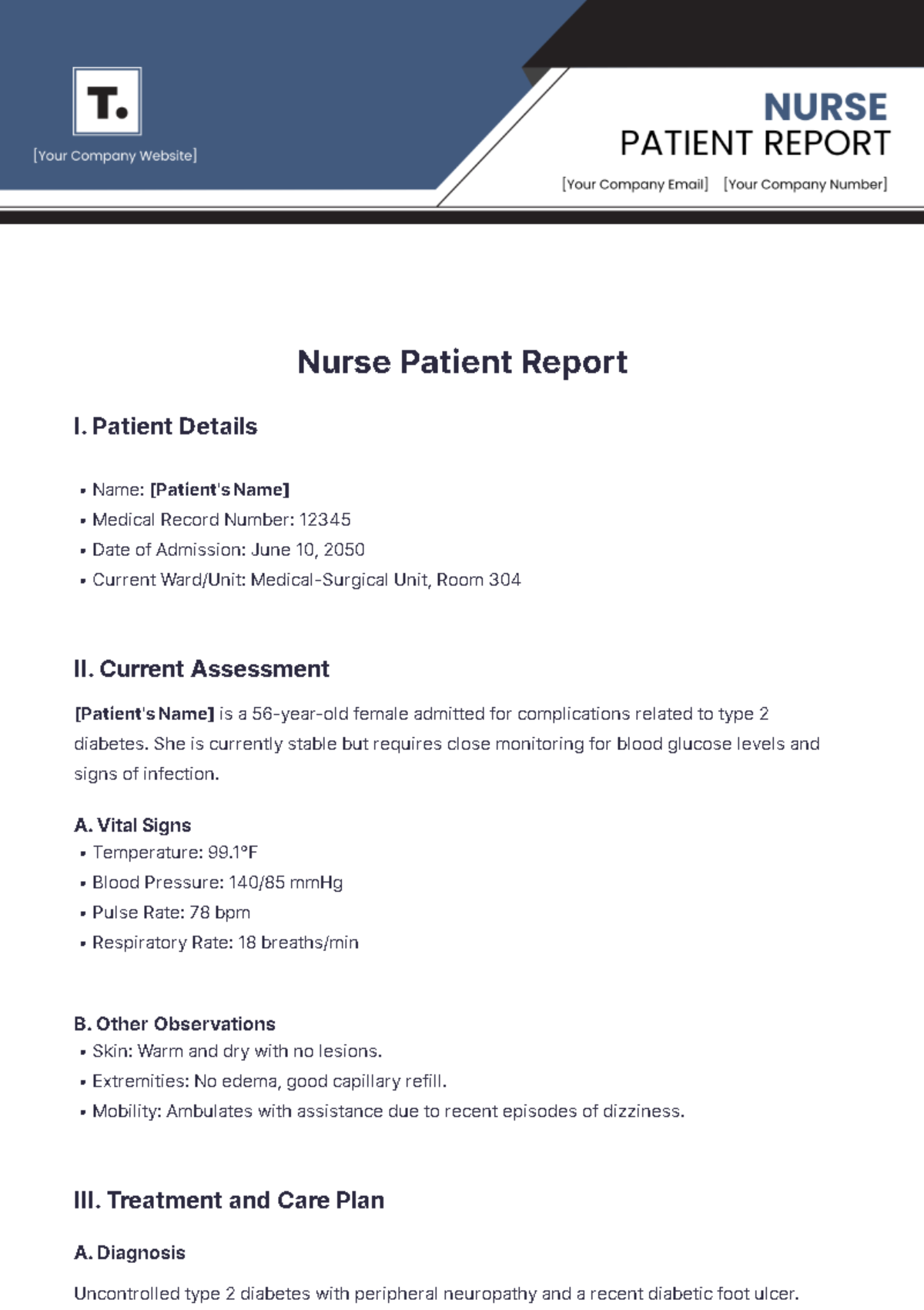
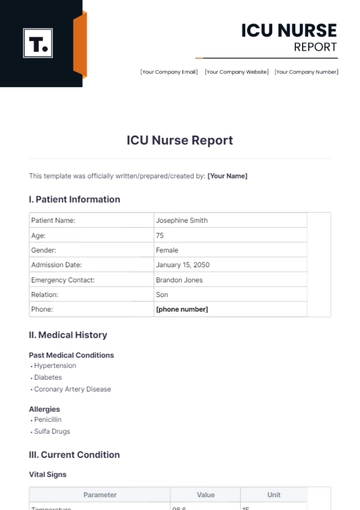
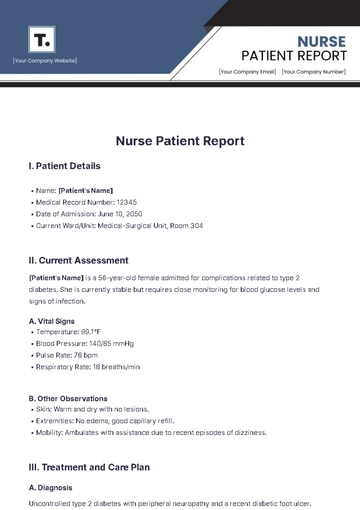
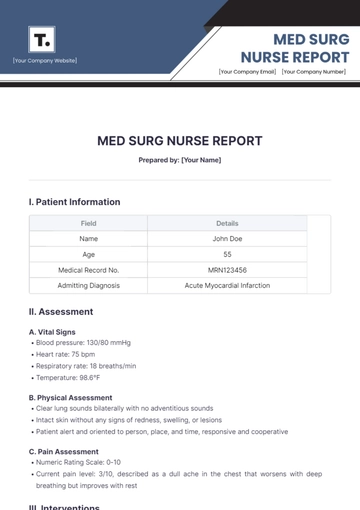
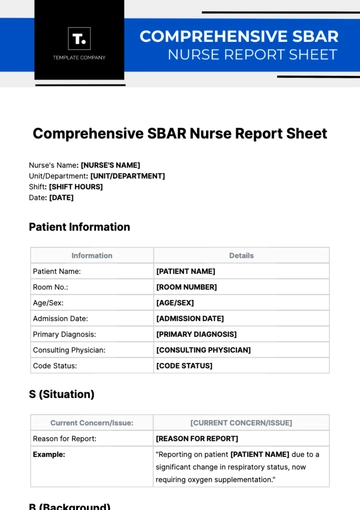
I. Patient Details
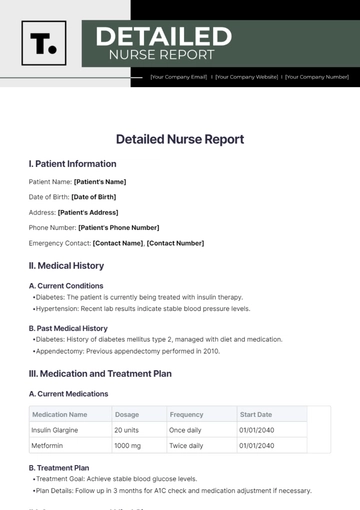
Name: [Patient's Name]
Medical Record Number: 12345
Date of Admission: June 10, 2050
Current Ward/Unit: Medical-Surgical Unit, Room 304
II. Current Assessment
[Patient's Name] is a 56-year-old female admitted for complications related to type 2 diabetes. She is currently stable but requires close monitoring for blood glucose levels and signs of infection.
A. Vital Signs
Temperature: 99.1°F
Blood Pressure: 140/85 mmHg
Pulse Rate: 78 bpm
Respiratory Rate: 18 breaths/min
B. Other Observations
Skin: Warm and dry with no lesions.
Extremities: No edema, good capillary refill.
Mobility: Ambulates with assistance due to recent episodes of dizziness.
III. Treatment and Care Plan
A. Diagnosis
Uncontrolled type 2 diabetes with peripheral neuropathy and a recent diabetic foot ulcer.
B. Medical Orders
Insulin therapy: Lantus 20 units at bedtime, Novolog sliding scale for meals.
Antibiotics: Ceftriaxone 1g IV every 24 hours for foot ulcer.
Wound care: Daily dressing changes with sterile technique.
Diet: Diabetic diet with calorie count monitoring.
Labs: Daily blood glucose levels, HbA1c, CBC, and BMP.
C. Nursing Interventions
Monitor blood glucose levels before meals and at bedtime.
Administer medications as per the schedule.
Perform wound care and monitor for signs of infection.
Assist with activities of daily living as needed.
IV. Medications
Lantus (Insulin Glargine) 20 units at bedtime
Novolog (Insulin Aspart) per sliding scale
Ceftriaxone 1g IV daily
Metformin 1000 mg BID
Lisinopril 10 mg daily
V. Patient Education
[Patient's Name] demonstrates good understanding of her care plan, asking relevant questions and expressing willingness to adhere to recommendations.
Key Teaching Points:
Importance of blood glucose monitoring and insulin administration.
Proper foot care techniques to prevent ulcers and infections.
Dietary recommendations for managing diabetes.
Recognition of hypoglycemia and hyperglycemia symptoms.
VI. Collaboration and Communication
A. Interdisciplinary Team
Primary Care Physician: Dr. [Name]
Endocrinologist: Dr. [Name]
Wound Care Specialist: [Name]
Dietitian: [Name]
B. Handover Notes
Ensure continuous monitoring of blood glucose levels and adjust insulin doses as needed.
Continue current antibiotic regimen and monitor for signs of infection.
Provide patient education on discharge planning and follow-up care.
VII. Summary and Recommendations
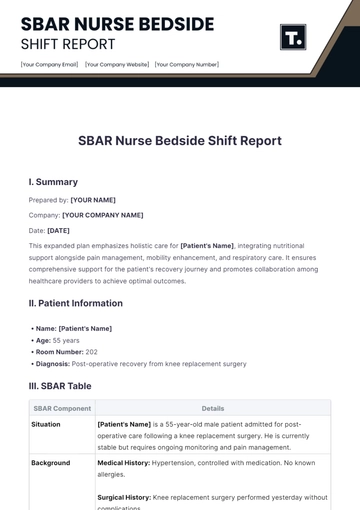
[Patient's Name] has shown gradual improvement since admission. Her blood glucose levels are stabilizing, and the foot ulcer is responding to treatment. The priority for the next shift includes maintaining strict glucose monitoring, continuing with the wound care regimen, and reinforcing patient education on diabetes management. Encourage ambulation with assistance to enhance mobility and prevent complications.
Prepared by:

[Your Name], RN
[Date]
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
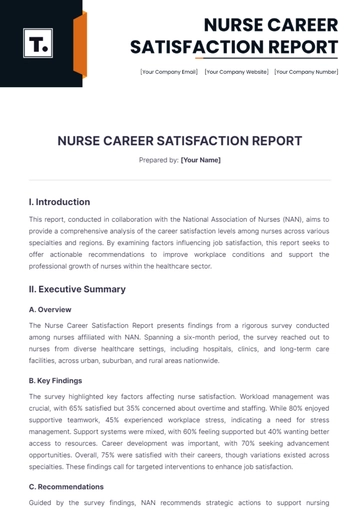
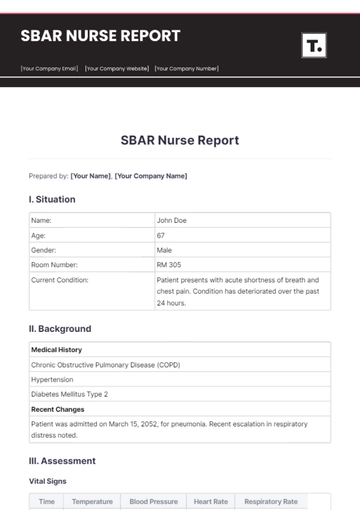
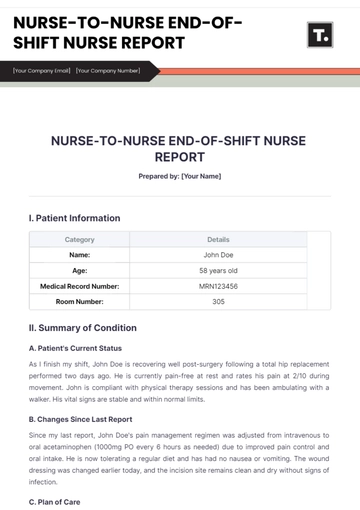
Improve patient care and communication with the Nurse Patient Report Template offered by Template.net. This customizable and downloadable template is designed to help nurses efficiently document patient interactions and medical information. Printable and editable in our AI Editor Tool, it ensures accurate and comprehensive reporting, making it easier to monitor patient progress and maintain high standards of care.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report