Free SBAR Nursing Worksheet
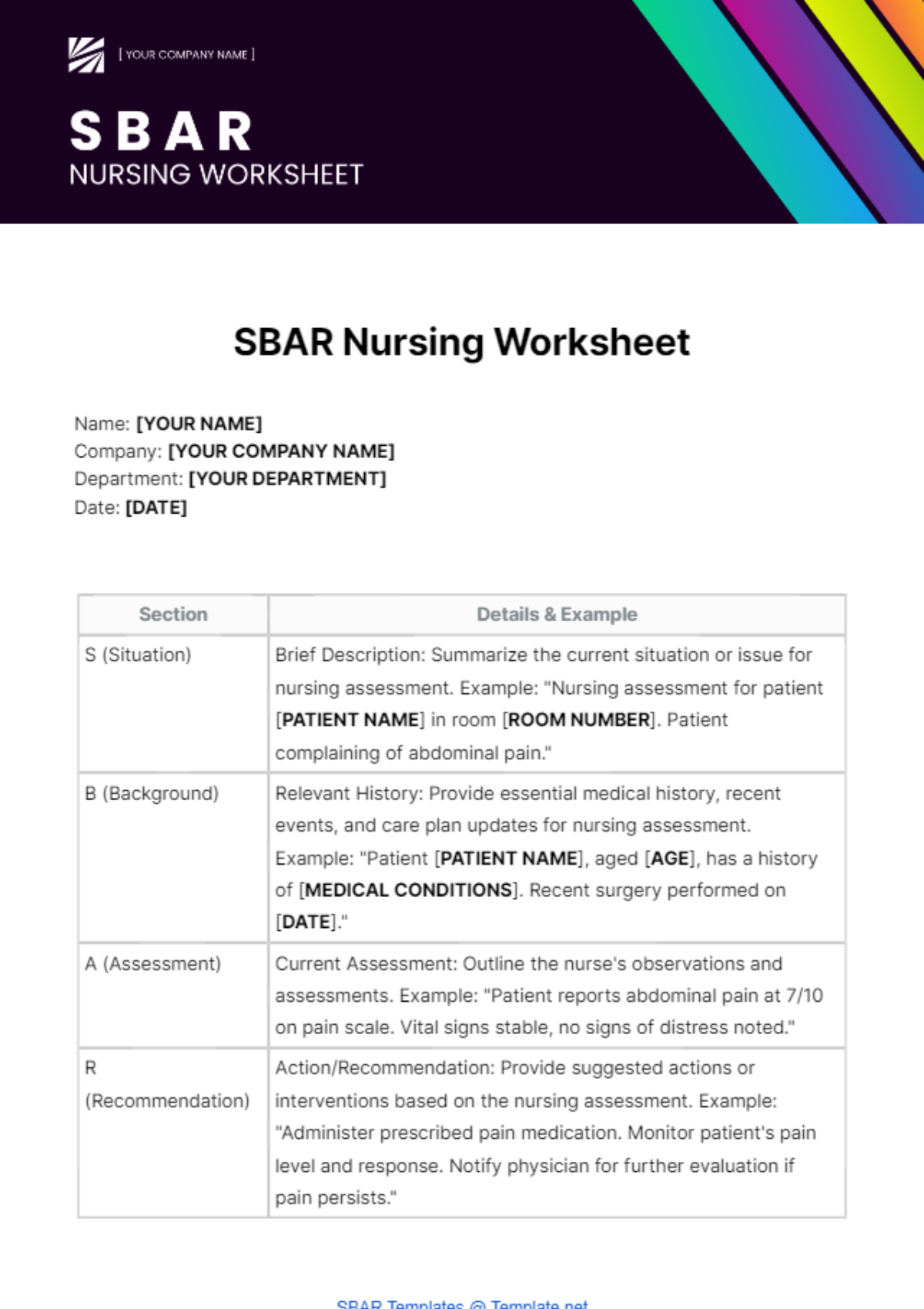
Name: [YOUR NAME]
Company: [YOUR COMPANY NAME]
Department: [YOUR DEPARTMENT]
Date: [DATE]
Section | Details & Example |
|---|---|
S (Situation) | Brief Description: Summarize the current situation or issue for nursing assessment. Example: "Nursing assessment for patient [PATIENT NAME] in room [ROOM NUMBER]. Patient complaining of abdominal pain." |
B (Background) | Relevant History: Provide essential medical history, recent events, and care plan updates for nursing assessment. Example: "Patient [PATIENT NAME], aged [AGE], has a history of [MEDICAL CONDITIONS]. Recent surgery performed on [DATE]." |
A (Assessment) | Current Assessment: Outline the nurse's observations and assessments. Example: "Patient reports abdominal pain at 7/10 on pain scale. Vital signs stable, no signs of distress noted." |
R (Recommendation) | Action/Recommendation: Provide suggested actions or interventions based on the nursing assessment. Example: "Administer prescribed pain medication. Monitor patient's pain level and response. Notify physician for further evaluation if pain persists." |
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the SBAR Nursing Worksheet Template, exclusively from Template.net. This editable and customizable tool streamlines communication in healthcare settings. Crafted for efficiency, it's editable in our Ai Editor Tool, ensuring seamless adaptation to diverse needs. Elevate your nursing workflow with this essential resource.
You may also like
- Attendance Sheet
- Work Sheet
- Sheet Cost
- Expense Sheet
- Tracker Sheet
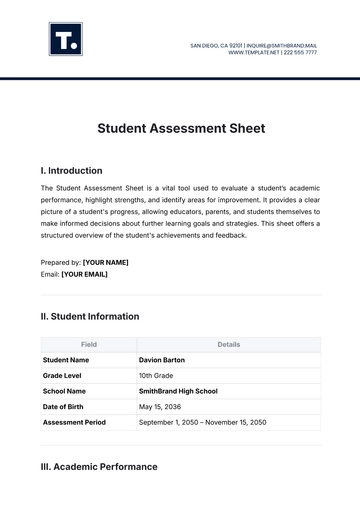
- Student Sheet
- Tracking Sheet
- Blank Sheet
- Information Sheet
- Sales Sheet
- Record Sheet
- Price Sheet
- Plan Sheet
- Score Sheet
- Estimate Sheet
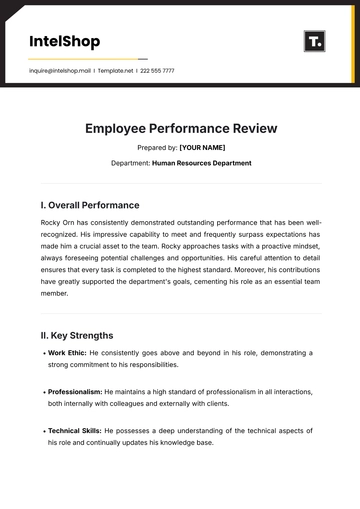
- Evaluation Sheet
- Checklist Sheet
- Bid Sheet
- Call Log Sheet
- Bill Sheet
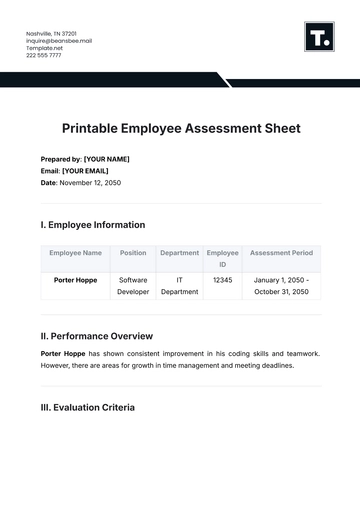
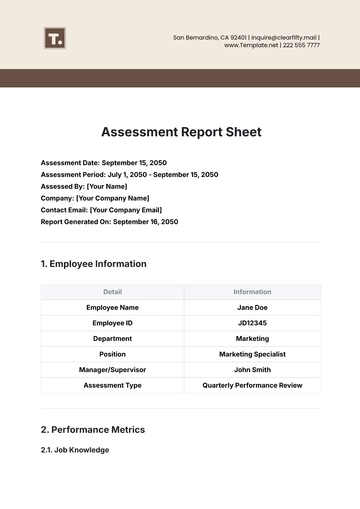
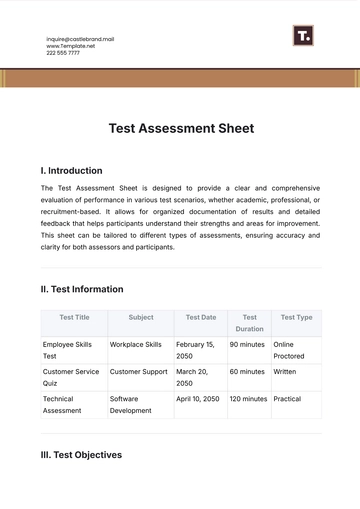
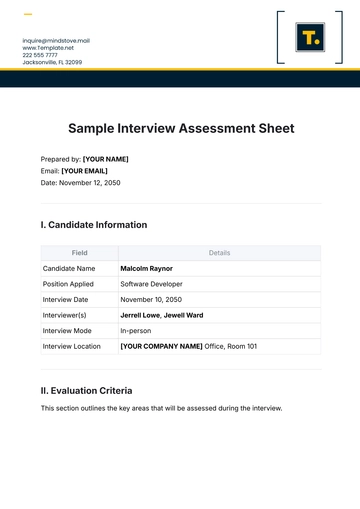
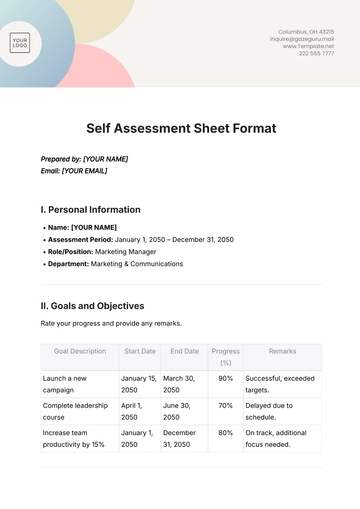
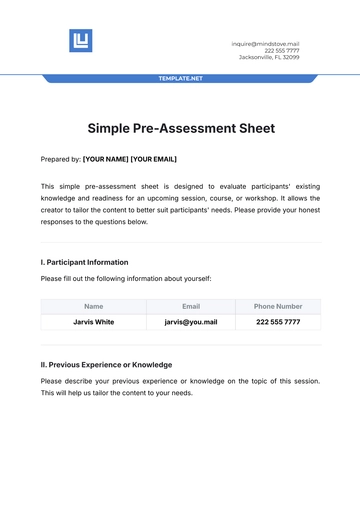
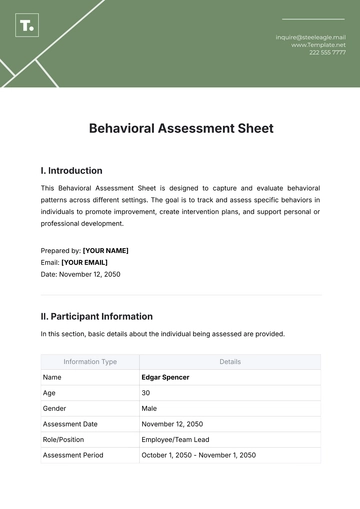
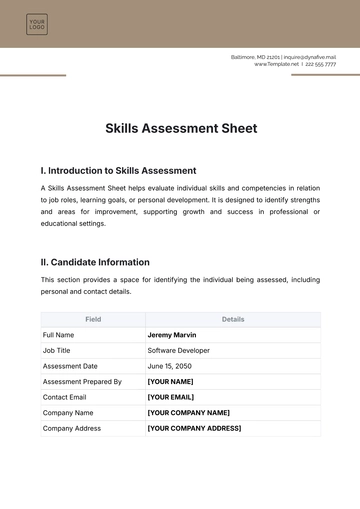
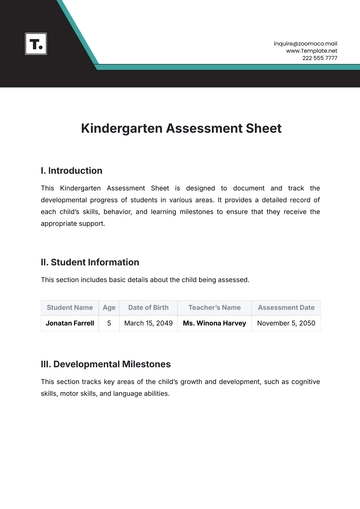
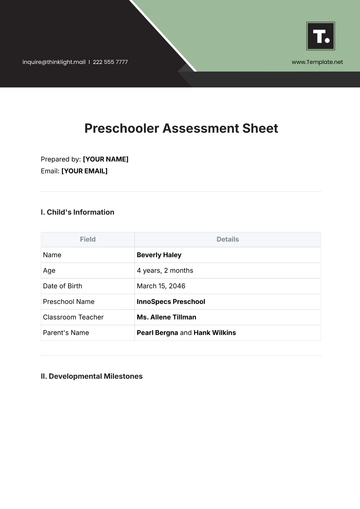
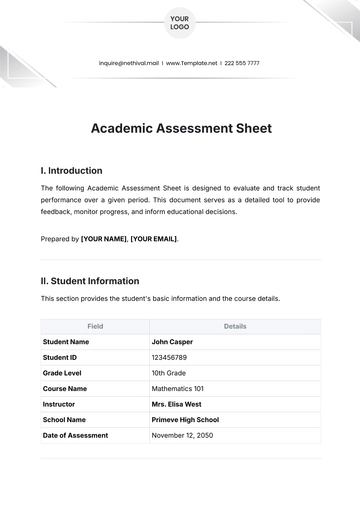
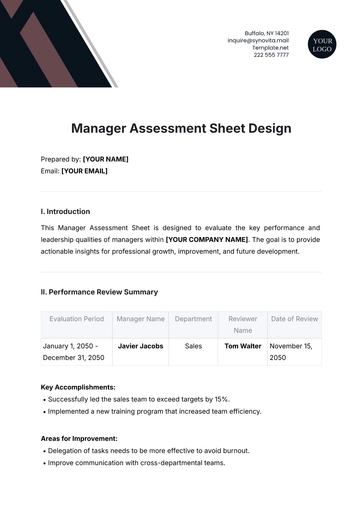
- Assessment Sheet
- Task Sheet
- School Sheet
- Work From Home Sheet
- Summary Sheet
- Construction Sheet
- Cover Sheet
- Debt Spreadsheet
- Debt Sheet
- Client Information Sheet
- University Sheet
- Freelancer Sheet
- Bookkeeping Sheet
- Itinerary Spreadsheet
- Scorecard Sheet
- Run Sheet
- Monthly Timesheet
- Event Sheet
- Advertising Agency Sheet
- Missing Numbers Worksheet
- Training Sheet
- Production Sheet
- Mortgage Sheet
- Answer Sheet
- Excel Sheet