Free Nursing Home Psychosocial Assessment
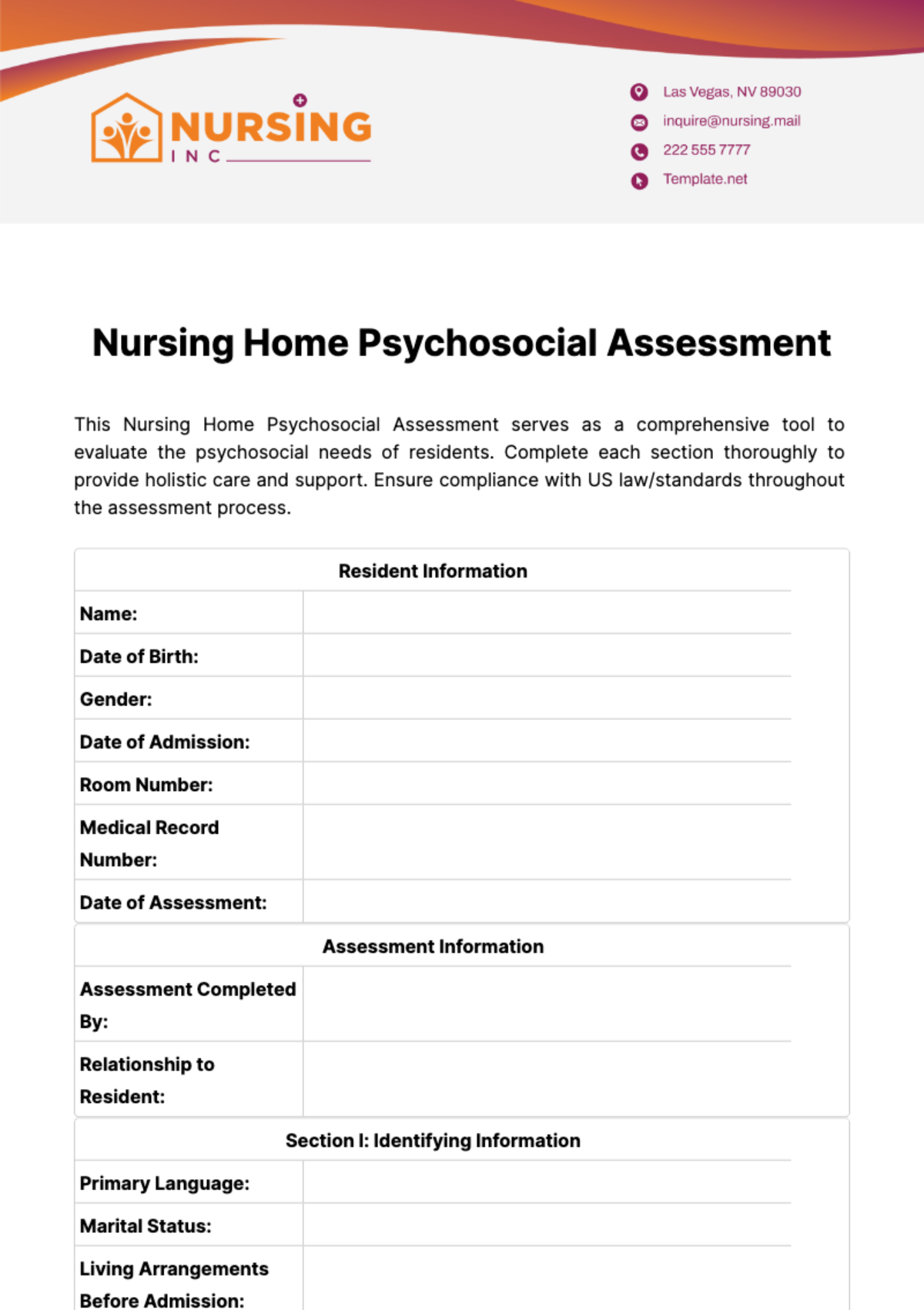
This Nursing Home Psychosocial Assessment serves as a comprehensive tool to evaluate the psychosocial needs of residents. Complete each section thoroughly to provide holistic care and support. Ensure compliance with US law/standards throughout the assessment process.
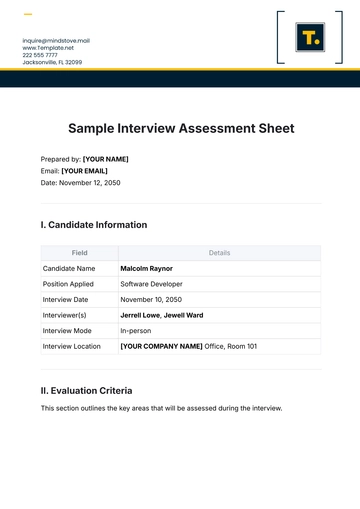
Resident Information | |
Name: | |
Date of Birth: | |
Gender: | |
Date of Admission: | |
Room Number: | |
Medical Record Number: | |
Date of Assessment: | |
Assessment Information | |
Assessment Completed By: | |
Relationship to Resident: | |
Section I: Identifying Information | |
Primary Language: | |
Marital Status: | |
Living Arrangements Before Admission: | |
Religion/Spiritual Preference: | |
Ethnicity/Race: | |
Occupation: | |
Section II: Medical History | |
Primary Diagnosis: | |
Other Medical Diagnoses/Conditions: | |
Allergies: | |
Current Medications: | |
Physician Information: | |
Section III: Social History | |
Family/Support System: | |
Living Situation Prior to Admission: | |
Educational Background: | |
Military Service: | |
Hobbies/Interests: | |
Financial Resources: | |
Section IV: Psychosocial Assessment | |
Mental Health History: | |
Cognitive Status: | |
Emotional Status: | |
Behavioral Observations: | |
Socialization Skills: | |
Support System: | |
Stressors/Concerns: | |
Coping Mechanisms: | |
Goals/Desires: | |
Section V: Environmental Assessment | |
Physical Environment: | |
Safety Concerns: | |
Accessibility: | |
Section VI: Recommendations/Plan of Care | |
Social Services Interventions: | |
Interdisciplinary Team Involvement: | |
Referrals: | |
Goals: | |
Plan of Action: | |
Section VII: Signatures

[Month, Day, Year]

[Month, Day, Year]
Confidentiality Statement: This document contains confidential information intended only for the use of the individual or entity to whom it is addressed. Unauthorized use, disclosure, or distribution is prohibited. If you are not the intended recipient, please notify the sender immediately and delete this document from your system.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Address comprehensive well-being with the Nursing Home Psychosocial Assessment Template from Template.net. This editable and customizable template enables detailed evaluation of residents' psychological and social needs, contributing to holistic care planning. Editable in our Ai Editor Tool, it's crucial for understanding individual resident backgrounds, preferences, and challenges, supporting their mental and emotional health in your nursing home environment.