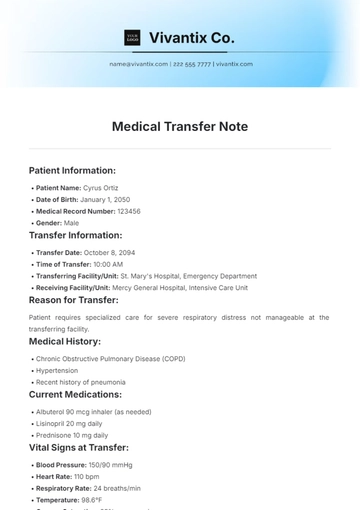
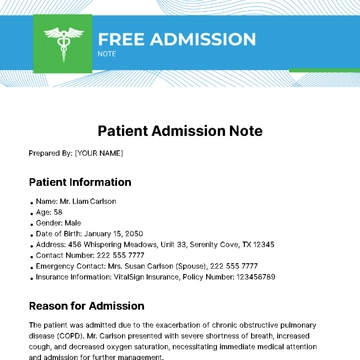
Free Patient Admission Note
Patient Name: Lawrence Orn
MRN: 123456789
Date of Admission: October 25, 2050
Attending Physician: Dr. [Your Name]
Consultants: None
Chief Complaint:
The patient presents with worsening shortness of breath and cough for the past three days.
History of Present Illness:
Lawrence Orn is a 39-year-old male with a history of asthma and seasonal allergies. He reports that his shortness of breath has progressively worsened over the last three days, associated with a non-productive cough and wheezing. He denies fever, chills, or chest pain. He has been using his rescue inhaler more frequently without significant relief.
Past Medical History:
Asthma
Seasonal allergies
Hypertension (controlled)
Medications:
Albuterol inhaler (as needed)
Lisinopril 10 mg daily
Allergies:
Penicillin (rash)
Family History:
Mother with a history of asthma
Father with hypertension
Social History:
Non-smoker
Occasional alcohol use
Works as a software engineer
Review of Systems:
Respiratory: Shortness of breath, wheezing.
Cardiovascular: No chest pain or palpitations.
Gastrointestinal: No nausea or vomiting.
Neurological: No headaches or dizziness.
Physical Examination:
Vital Signs: BP 130/85 mmHg, HR 88 bpm, RR 22 breaths/min, Temp 98.6°F, SpO2 92% on room air.
General: Alert and oriented, in mild respiratory distress.
HEENT: Clear nasal passages, no oropharyngeal edema.
Respiratory: Decreased breath sounds bilaterally, wheezing on expiration.
Cardiovascular: Regular rate and rhythm, no murmurs.
Abdomen: Soft, non-tender, no distension.
Extremities: No edema, capillary refill < 2 seconds.
Assessment:
Asthma exacerbation.
Possible viral bronchitis.
Plan:
Administer nebulized albuterol and ipratropium bromide in the ER.
Obtain a chest X-ray to rule out pneumonia.
Start oral prednisone 40 mg daily for 5 days.
Monitor vital signs and respiratory status.
Consult pulmonary if no improvement in 24 hours.
Educate the patient on asthma management and the importance of medication adherence.
Schedule follow-up in 1 week.
Signature:

Dr. [Your Name], MD
Date: October 25, 2050
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline patient documentation with Template.net’s Patient Admission Note Template. Fully customizable and editable, this template ensures easy data entry and accurate records. Editable in our AI Editor Tool, it’s perfect for healthcare professionals needing efficiency and flexibility in managing patient information. Save time and maintain consistency with this versatile, user-friendly tool.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note