Free General Practitioner Hospital Note
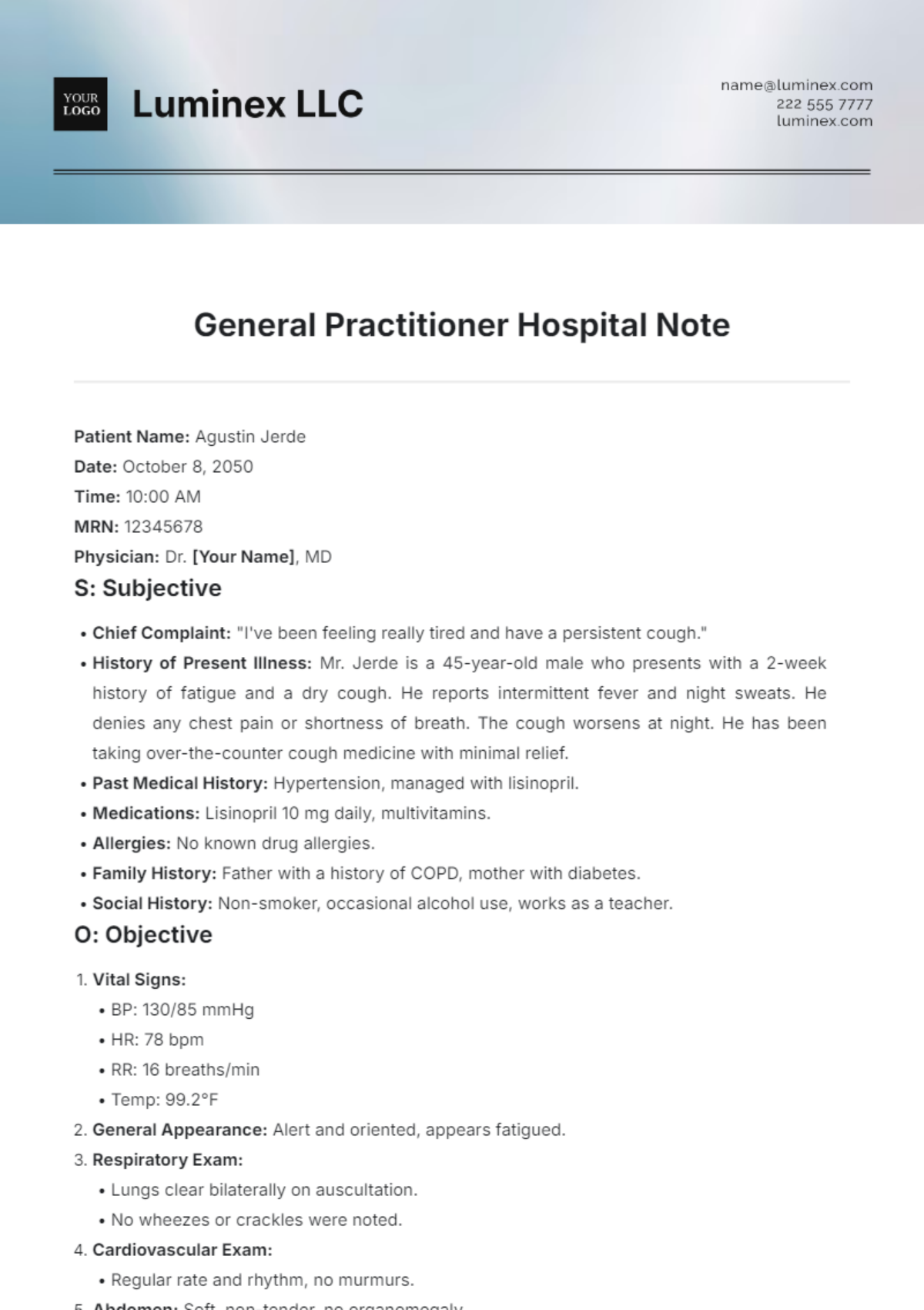
Patient Name: Agustin Jerde
Date: October 8, 2050
Time: 10:00 AM
MRN: 12345678
Physician: Dr. [Your Name], MD
S: Subjective
Chief Complaint: "I've been feeling really tired and have a persistent cough."
History of Present Illness: Mr. Jerde is a 45-year-old male who presents with a 2-week history of fatigue and a dry cough. He reports intermittent fever and night sweats. He denies any chest pain or shortness of breath. The cough worsens at night. He has been taking over-the-counter cough medicine with minimal relief.
Past Medical History: Hypertension, managed with lisinopril.
Medications: Lisinopril 10 mg daily, multivitamins.
Allergies: No known drug allergies.
Family History: Father with a history of COPD, mother with diabetes.
Social History: Non-smoker, occasional alcohol use, works as a teacher.
O: Objective
Vital Signs:
BP: 130/85 mmHg
HR: 78 bpm
RR: 16 breaths/min
Temp: 99.2°F
General Appearance: Alert and oriented, appears fatigued.
Respiratory Exam:
Lungs clear bilaterally on auscultation.
No wheezes or crackles were noted.
Cardiovascular Exam:
Regular rate and rhythm, no murmurs.
Abdomen: Soft, non-tender, no organomegaly.
Skin: No rashes or lesions.
A: Assessment
Fatigue and dry cough, likely viral etiology. Consideration of possible bronchitis or upper respiratory infection. Differential diagnoses include:
Viral upper respiratory infection
Bacterial bronchitis
Pneumonia (less likely given lung exam findings)
P: Plan
Lab Tests:
CBC to assess for infection.
Chest X-ray if symptoms persist or worsen.
Medications:
Prescribe a cough suppressant (dextromethorphan) for symptom relief.
Advise hydration and rest.
Follow-Up:
Return in one week or sooner if symptoms worsen (e.g., difficulty breathing, high fever).
Patient Education:
Educate about the signs of dehydration and when to seek immediate care.
Discuss the importance of hand hygiene and avoiding close contact with sick individuals.
Signature:

Dr. [Your Name], MD
General Practitioner
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline your patient documentation with the General Practitioner Hospital Note Template from Template.net. This editable template allows for seamless customization to fit your specific needs. Easily modify and personalize each section using our AI Editor Tool, ensuring your notes are both efficient and tailored to your practice. Enhance your workflow today!
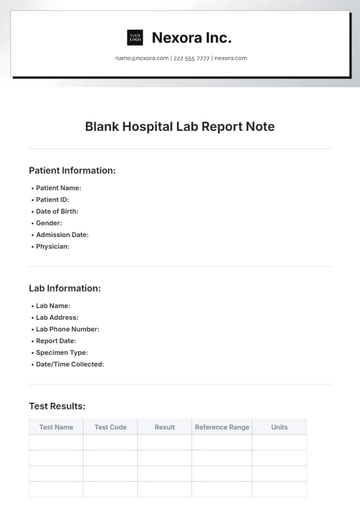
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note