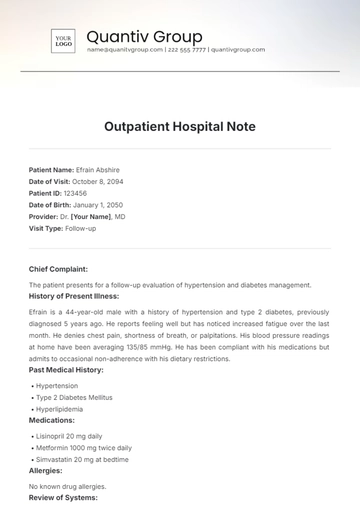
Free Outpatient Hospital Note
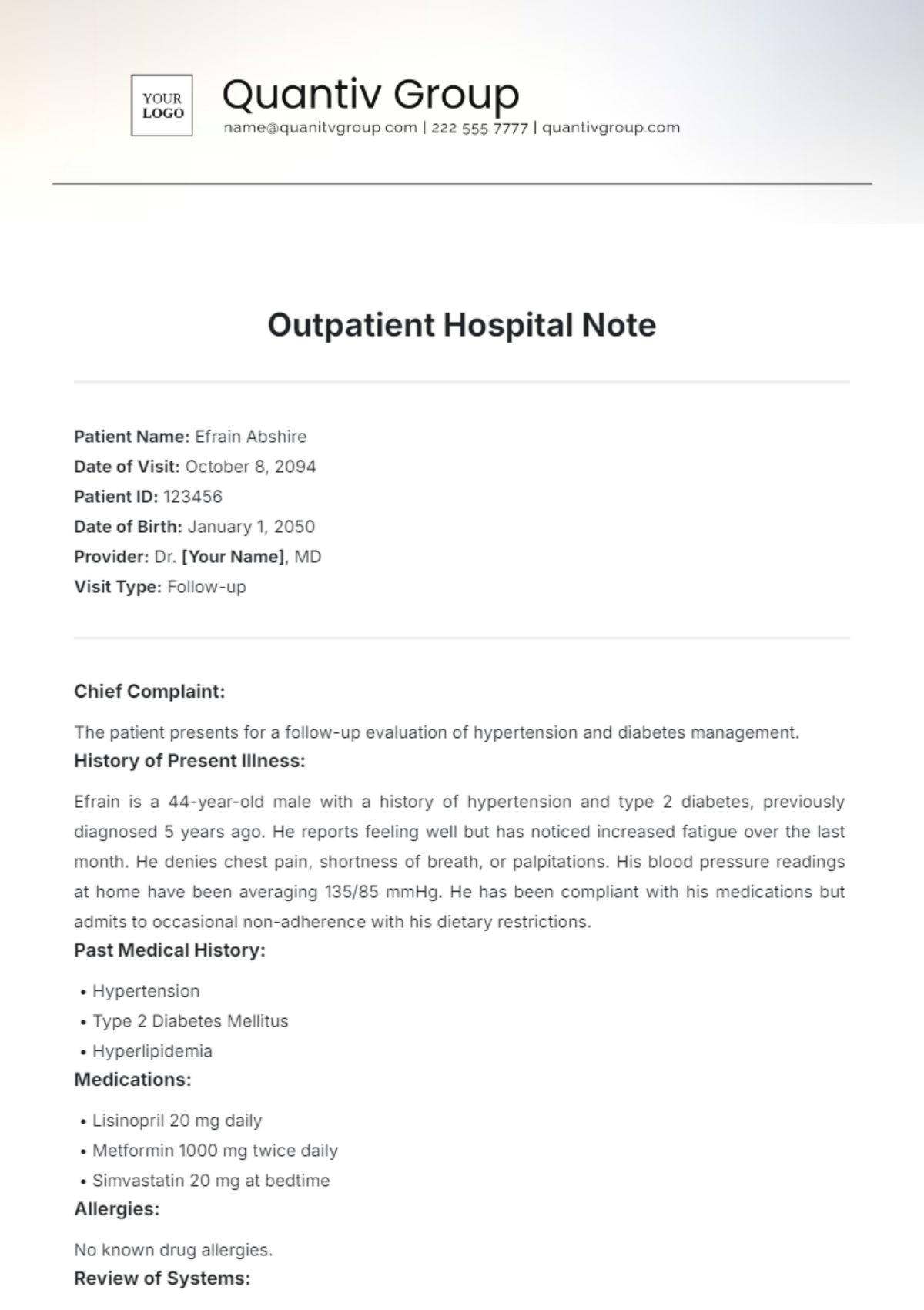
Patient Name: Efrain Abshire
Date of Visit: October 8, 2094
Patient ID: 123456
Date of Birth: January 1, 2050
Provider: Dr. [Your Name], MD
Visit Type: Follow-up
Chief Complaint:
The patient presents for a follow-up evaluation of hypertension and diabetes management.
History of Present Illness:
Efrain is a 44-year-old male with a history of hypertension and type 2 diabetes, previously diagnosed 5 years ago. He reports feeling well but has noticed increased fatigue over the last month. He denies chest pain, shortness of breath, or palpitations. His blood pressure readings at home have been averaging 135/85 mmHg. He has been compliant with his medications but admits to occasional non-adherence with his dietary restrictions.
Past Medical History:
Hypertension
Type 2 Diabetes Mellitus
Hyperlipidemia
Medications:
Lisinopril 20 mg daily
Metformin 1000 mg twice daily
Simvastatin 20 mg at bedtime
Allergies:
No known drug allergies.
Review of Systems:
Cardiovascular: No chest pain or palpitations.
Respiratory: No shortness of breath or cough.
Endocrine: Increased fatigue.
Gastrointestinal: No changes in bowel habits or abdominal pain.
Genitourinary: No urinary issues.
Physical Exam:
Vital Signs:
Blood Pressure: 130/80 mmHg
Heart Rate: 72 bpm
Respiratory Rate: 16 breaths/min
Weight: 200 lbs
Height: 5'10"
General: Alert and oriented, in no acute distress.
Cardiovascular: Regular rate and rhythm, no murmurs.
Respiratory: Clear to auscultation bilaterally.
Abdomen: Soft, non-tender, no organomegaly.
Extremities: No edema.
Assessment:
Hypertension: Well-controlled.
Type 2 Diabetes Mellitus: Stable but needs dietary reinforcement.
Fatigue: Likely related to lifestyle factors and possible medication side effects.
Plan:
Continue current medications.
Reinforce dietary modifications; consider referral to a dietitian.
Schedule a follow-up appointment in 3 months for monitoring.
Educate the patient on the signs of hypoglycemia.
Consider hemoglobin A1c testing at the next visit.
Patient Education:
Discussed the importance of diet, exercise, and medication adherence. Provided educational materials on diabetes management.
Signature:

Dr. [Your Name], MD
October 8, 2094
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Elevate your documentation with the Outpatient Hospital Note Template from Template.net. This customizable and editable template streamlines your patient records, ensuring accuracy and efficiency. With our AI Editor Tool, you can effortlessly tailor the notes to fit your needs, making it easier to provide top-notch patient care while saving valuable time. Perfect for any healthcare professional!
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
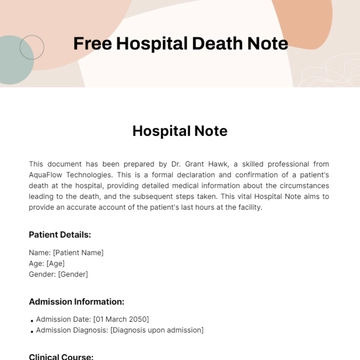
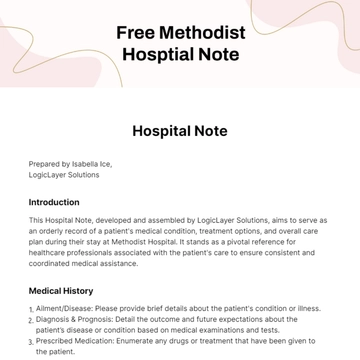
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note