Free Family Medicine Soap Note
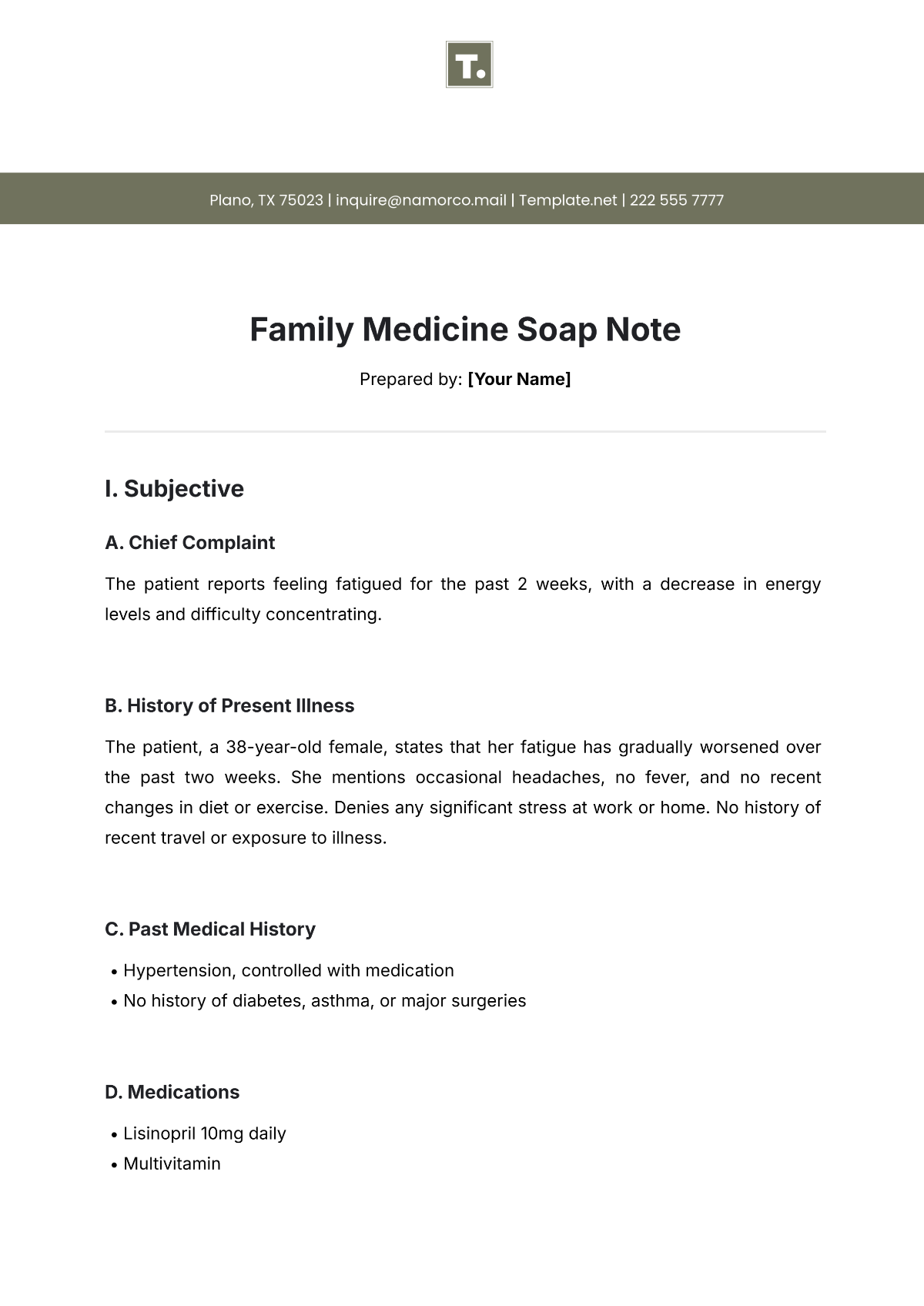
Prepared by: [Your Name]
I. Subjective
A. Chief Complaint
The patient reports feeling fatigued for the past 2 weeks, with a decrease in energy levels and difficulty concentrating.
B. History of Present Illness
The patient, a 38-year-old female, states that her fatigue has gradually worsened over the past two weeks. She mentions occasional headaches, no fever, and no recent changes in diet or exercise. Denies any significant stress at work or home. No history of recent travel or exposure to illness.
C. Past Medical History
Hypertension, controlled with medication
No history of diabetes, asthma, or major surgeries
D. Medications
Lisinopril 10mg daily
Multivitamin
E. Allergies
No known drug allergies (NKDA)
F. Family History
Mother: Hypertension, type 2 diabetes
Father: Heart disease, deceased at 65
G. Social History
Non-smoker
Social drinker (1-2 glasses of wine per week)
Works as a marketing manager from home
H. Review of Systems
General: Reports fatigue and low energy
Cardiovascular: No chest pain or palpitations
Respiratory: No shortness of breath or cough
Neurological: Occasional headaches, no dizziness or syncope
II. Objective
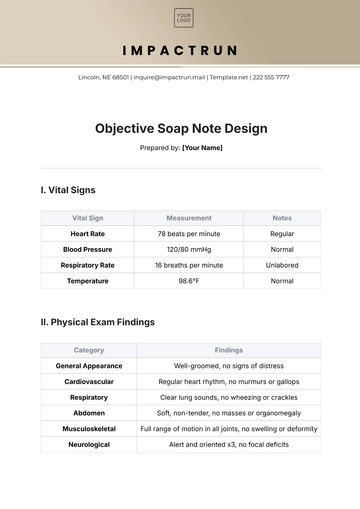
A. Vital Signs
Vital Sign | Measurement |
|---|---|
Blood Pressure | 130/85 mmHg |
Heart Rate | 72 bpm, regular |
Respiratory Rate | 16 breaths/min |
Temperature | 98.6°F (37°C) |
Oxygen Saturation | 98% on room air |
Weight | 160 lbs |
Height | 5'6" |
B. Physical Examination
System | Findings |
|---|---|
General | Well-appearing, alert, and oriented to time, place, and person |
HEAT | No signs of sinus tenderness, no swollen lymph nodes, oral mucosa moist |
Cardiovascular | Regular rhythm, no murmurs or gallops, normal peripheral pulses |
Respiratory | Clear to auscultation bilaterally, no wheezes or crackles |
Abdomen | Soft, non-tender, no hepatosplenomegaly |
Neurological | Cranial nerves intact, no focal deficits, normal strength, and sensation in all limbs |
Skin | No rashes or lesions |
C. Laboratory Results
Test | Result | Normal Range |
|---|---|---|
Complete Blood Count (CBC) | ||
White Blood Cell (WBC) | 5,000/mm³ | 4,000-11,000/mm³ |
Hemoglobin | 13.5 g/dL | 12-16 g/dL (female) |
Platelets | 250,000/mm³ | 150,000-450,000/mm³ |
Thyroid-stimulating hormone (TSH) | 3.2 µIU/mL | 0.4-4.0 µIU/mL |
Comprehensive Metabolic Panel | Within normal limits |
III. Assessment
The patient presents with fatigue that has gradually worsened over the past two weeks. There are no signs of acute illness or concerning neurological symptoms. The most likely differential diagnoses include:
Primary Diagnosis: Fatigue likely related to stress or mild depression
Secondary Diagnosis: Possible anemia or early hypothyroidism (though lab results are normal)
IV. Plan
A. Diagnostic Plan
Continue monitoring vital signs and review lab results at follow-up
Consider ordering iron studies or a sleep study if symptoms persist
B. Therapeutic Plan
Recommend daily exercise (e.g., walking 30 minutes/day)
Encourage good sleep hygiene and stress management techniques
C. Follow-up Plan
Follow up in 2 weeks to reassess fatigue and discuss the results of any additional tests.
Schedule a mental health assessment if fatigue persists without a clear cause.
D. Patient Education
Advised the patient on the importance of regular exercise, sleep, and stress management
Provided handouts on improving sleep hygiene and managing stress
E. Referrals
None at this time, unless symptoms worsen or persist.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline patient care in your practice with Template.net's Family Medicine Soap Note Template. This editable, customizable template is perfect for family physicians. Efficiently document patient encounters using our Ai Editor Tool, ensuring comprehensive, precise notes that enhance continuity of care and patient outcomes.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note