Free Family Practice Soap Note
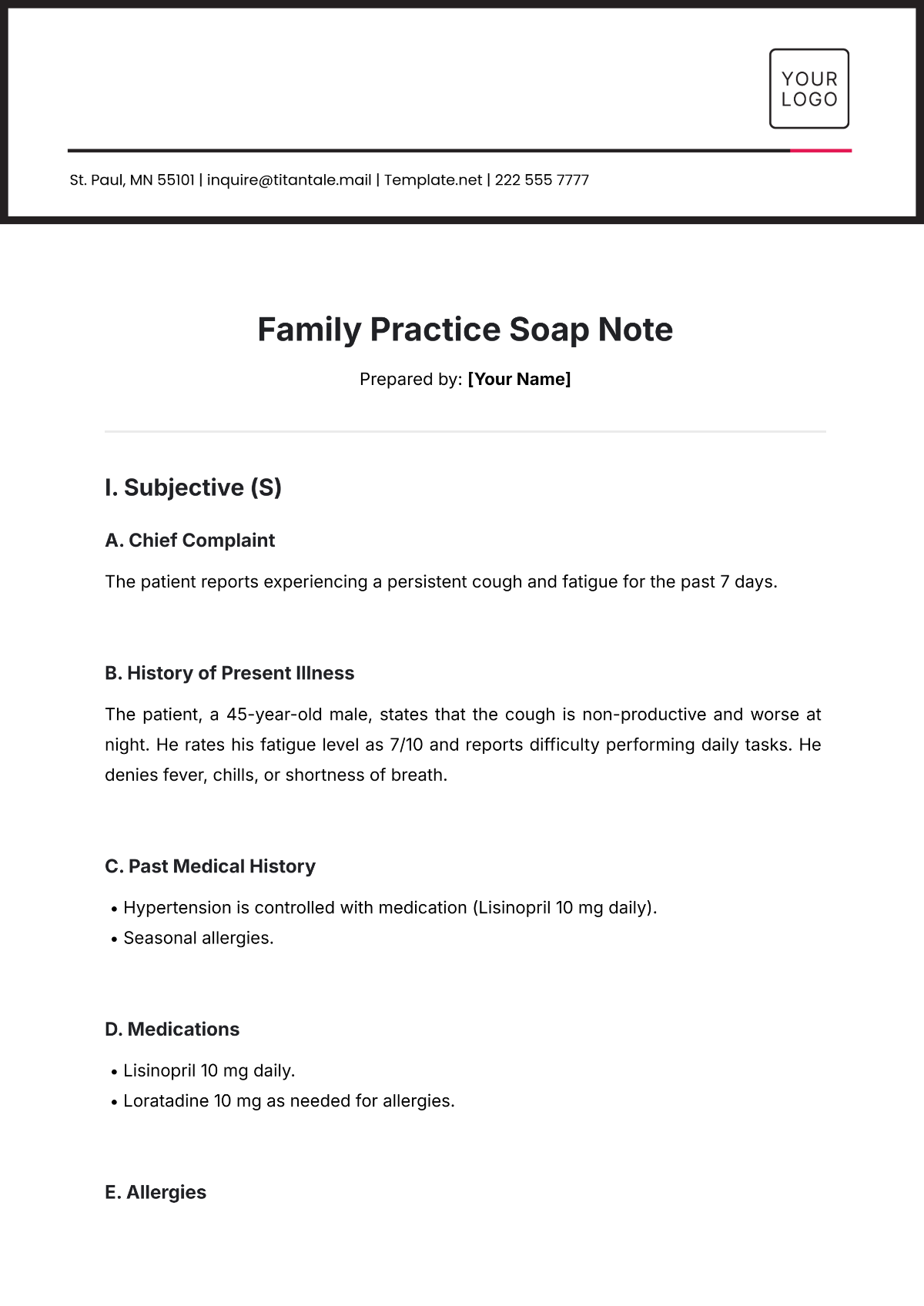
Prepared by: [Your Name]
I. Subjective (S)
A. Chief Complaint
The patient reports experiencing a persistent cough and fatigue for the past 7 days.
B. History of Present Illness
The patient, a 45-year-old male, states that the cough is non-productive and worse at night. He rates his fatigue level as 7/10 and reports difficulty performing daily tasks. He denies fever, chills, or shortness of breath.
C. Past Medical History
Hypertension is controlled with medication (Lisinopril 10 mg daily).
Seasonal allergies.
D. Medications
Lisinopril 10 mg daily.
Loratadine 10 mg as needed for allergies.
E. Allergies
Penicillin (rash).
F. Social History
Non-smoker, no alcohol use.
Works as an accountant with, a sedentary lifestyle.
G. Family History
Father: Hypertension.
Mother: Diabetes type 2.
II. Objective (O)
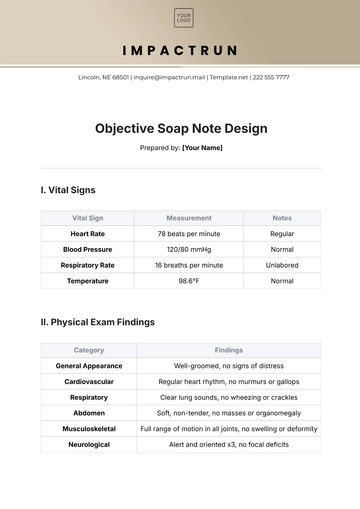
A. Vital Signs
Blood Pressure: 128/84 mmHg.
Heart Rate: 78 bpm.
Respiratory Rate: 18 breaths/min.
Temperature: 98.6°F.
Oxygen Saturation: 97% on room air.
B. Physical Examination
General Appearance: Alert and oriented, appears slightly tired.
HEENT: No nasal discharge, throat mildly erythematous without exudates.
Lungs: Clear to auscultation bilaterally, no wheezes or crackles.
Cardiovascular: Regular rhythm, no murmurs.
Abdomen: Soft, non-tender, no masses.
Extremities: No edema.
C. Diagnostic Results
Rapid COVID-19 test: Negative.
Chest X-ray: Pending.
III. Assessment (A)
Likely a viral upper respiratory infection (URI).
Fatigue related to viral illness or sedentary lifestyle.
Hypertension is controlled.
IV. Plan (P)
A. Medications
Prescribed guaifenesin 200 mg twice daily for symptomatic relief.
Advised to continue Lisinopril and Loratadine as directed.
B. Diagnostics
Awaiting chest X-ray results.
C. Patient Education
Encouraged increased fluid intake and rest.
Discussed the importance of physical activity and considering a mild exercise routine once symptoms resolve.
D. Follow-Up
Return in 7 days or sooner if symptoms worsen or new symptoms develop.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Streamline your family practice with Template.net's Family Practice Soap Note Template. Customizable and editable, this tool is designed to enhance patient records with efficiency and precision. Utilize our Ai Editor Tool to tailor each note to your practice's needs, ensuring optimal patient care and streamlined documentation.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note