Free Speech Therapy Soap Note
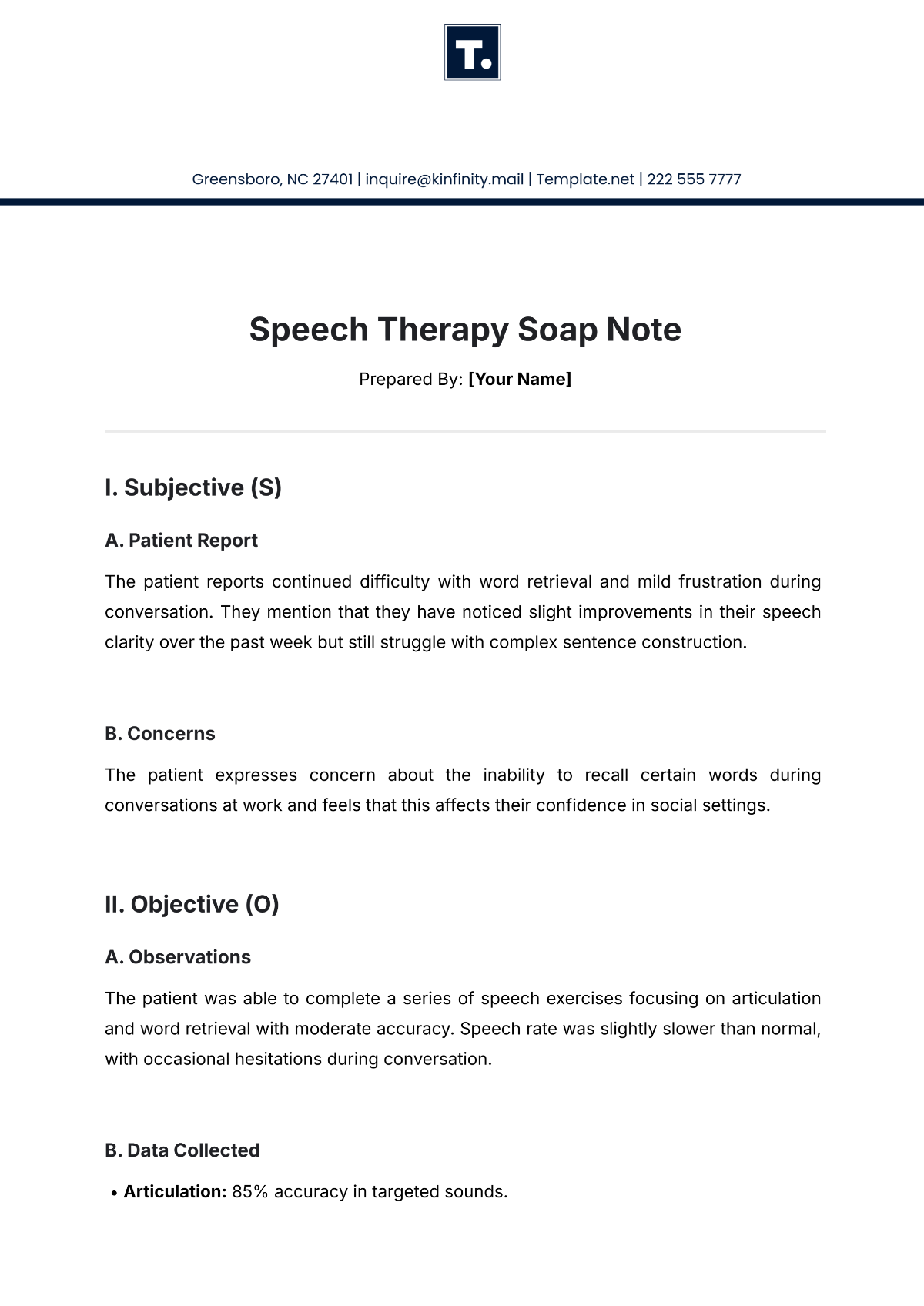
Prepared By: [Your Name]
I. Subjective (S)
A. Patient Report
The patient reports continued difficulty with word retrieval and mild frustration during conversation. They mention that they have noticed slight improvements in their speech clarity over the past week but still struggle with complex sentence construction.
B. Concerns
The patient expresses concern about the inability to recall certain words during conversations at work and feels that this affects their confidence in social settings.
II. Objective (O)
A. Observations
The patient was able to complete a series of speech exercises focusing on articulation and word retrieval with moderate accuracy. Speech rate was slightly slower than normal, with occasional hesitations during conversation.
B. Data Collected
Articulation: 85% accuracy in targeted sounds.
Word Retrieval: 70% accuracy in spontaneous speech tasks.
Sentence Structure: Mild difficulty in constructing sentences with appropriate grammar and complexity.
III. Assessment (A)
The patient has made slight progress in articulation but continues to experience moderate difficulty with word retrieval and sentence construction. Progress is slower than expected, possibly due to anxiety during communication, which may be impacting overall performance. The current treatment plan is partially effective, but more focus on anxiety-reducing strategies could be beneficial.
IV. Plan (P)
Continue with articulation exercises and word retrieval tasks in therapy sessions.
Introduce cognitive strategies to reduce anxiety during speaking situations.
Increase focus on sentence construction with both structured and unstructured tasks.
Review progress in two weeks and adjust treatment goals if necessary.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Enhance your therapeutic documentation with Template.net's Speech Therapy Soap Note Template. Designed for speech-language pathologists, this editable and customizable template streamlines patient progress tracking. Easily modify content to suit individual therapy sessions using our Ai Editor Tool, ensuring detailed and accurate notes every time.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note