Free Social Work Soap Note Outline
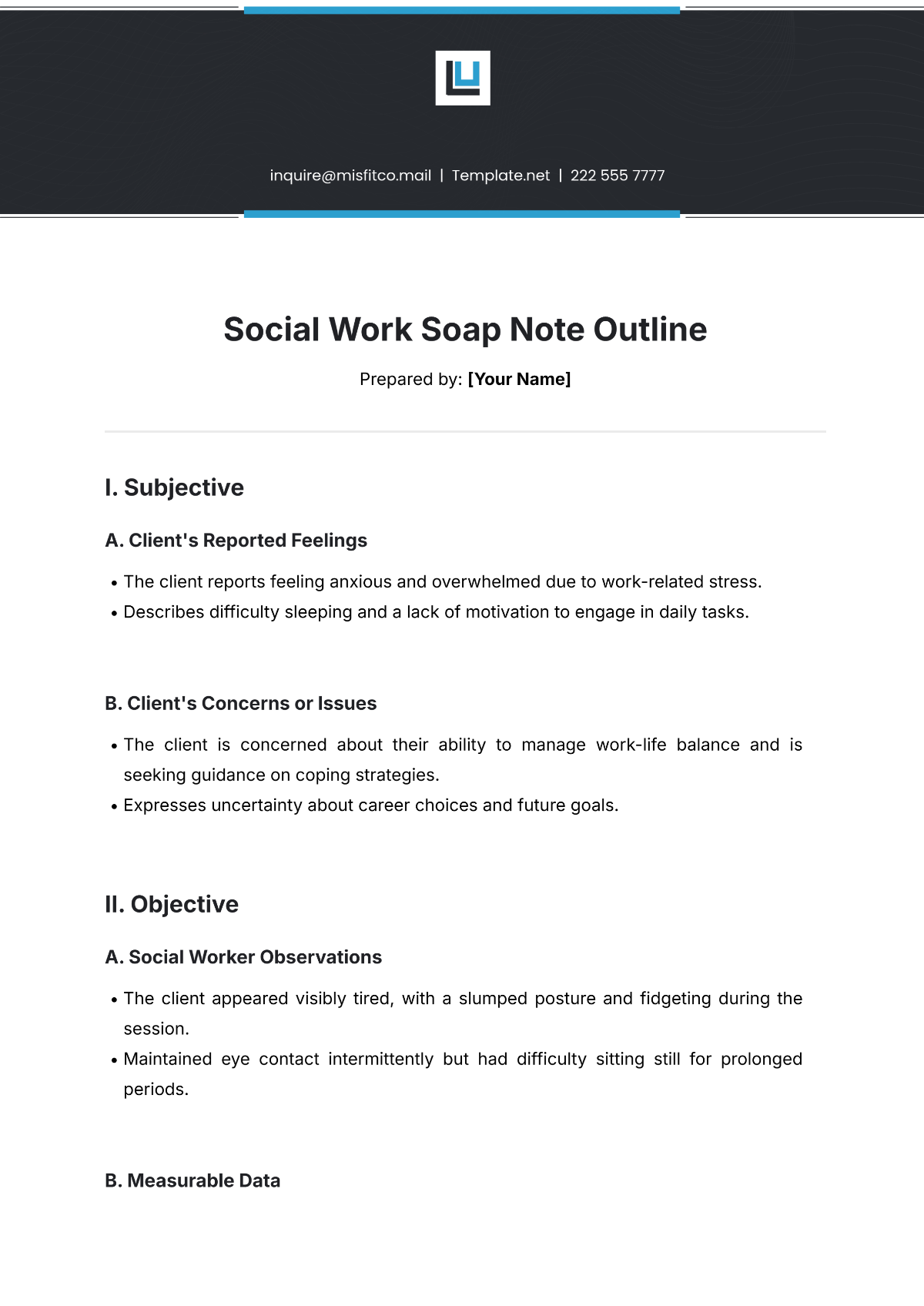
Prepared by: [Your Name]
I. Subjective
A. Client's Reported Feelings
The client reports feeling anxious and overwhelmed due to work-related stress.
Describes difficulty sleeping and a lack of motivation to engage in daily tasks.
B. Client's Concerns or Issues
The client is concerned about their ability to manage work-life balance and is seeking guidance on coping strategies.
Expresses uncertainty about career choices and future goals.
II. Objective
A. Social Worker Observations
The client appeared visibly tired, with a slumped posture and fidgeting during the session.
Maintained eye contact intermittently but had difficulty sitting still for prolonged periods.
B. Measurable Data
No significant changes in weight or health were reported since the last session.
Client's mood rating: 4/10 on a scale of 1 to 10.
III. Assessment
A. Social Worker’s Analysis
The client’s symptoms of anxiety appear to be related to ongoing work stress and a lack of coping mechanisms.
The client’s emotional state seems to have worsened due to recent challenges in the workplace.
B. Progress and Challenges
The client has demonstrated some progress in identifying stressors but still struggles to implement coping strategies discussed in previous sessions.
Difficulty engaging in self-care routines continues to be a barrier.
IV. Plan
A. Immediate Actions
Continue exploring stress management techniques, such as mindfulness and time management strategies.
Encourage the client to keep a daily journal to track feelings and identify triggers.
B. Long-Term Plan
Schedule a follow-up appointment in two weeks to assess progress and reassess the client’s coping strategies.
Consider referring the client to a career counselor if work-related issues persist.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Ensure thorough social work documentation with our Social Work SOAP Note Outline Template, offered by Template.net. This editable and customizable template provides a professional structure for capturing client details, assessments, and interventions. Adjust it effortlessly editable in our AI Editor Tool to suit your specific practice needs. Designed for social workers, this template simplifies the process of maintaining organized and accurate records while meeting professional standards.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note