Free Chest Pain Soap Note
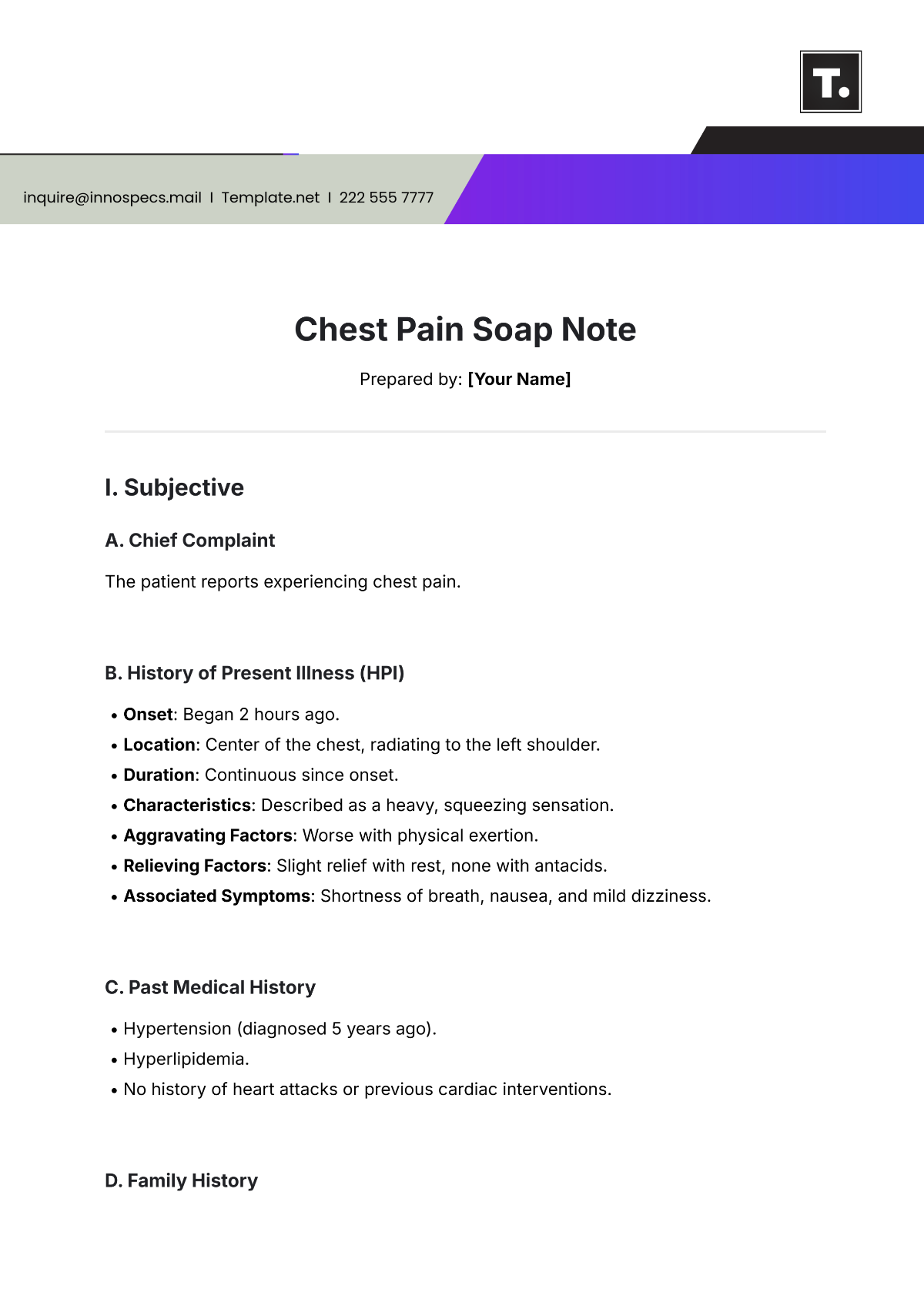
Prepared by: [Your Name]
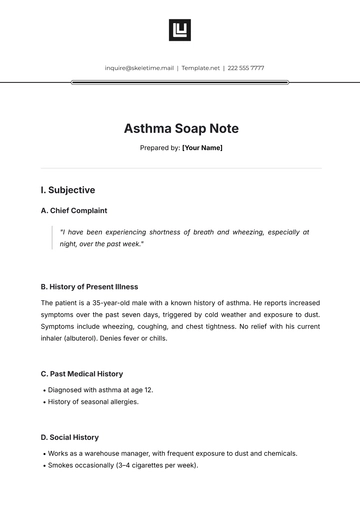
I. Subjective
A. Chief Complaint
The patient reports experiencing chest pain.
B. History of Present Illness (HPI)
Onset: Began 2 hours ago.
Location: Center of the chest, radiating to the left shoulder.
Duration: Continuous since onset.
Characteristics: Described as a heavy, squeezing sensation.
Aggravating Factors: Worse with physical exertion.
Relieving Factors: Slight relief with rest, none with antacids.
Associated Symptoms: Shortness of breath, nausea, and mild dizziness.
C. Past Medical History
Hypertension (diagnosed 5 years ago).
Hyperlipidemia.
No history of heart attacks or previous cardiac interventions.
D. Family History
Father: Died of a heart attack at age 58.
Mother: Diagnosed with type 2 diabetes.
F. Social History
Smoker: 10 cigarettes per day for 15 years.
Alcohol: Occasionally drinks on weekends.
Exercise: Sedentary lifestyle.
G. Review of Systems (ROS)
Cardiovascular: Reports chest tightness and palpitations.
Respiratory: No coughing or wheezing.
Gastrointestinal: No vomiting but has nausea.
II. Objective
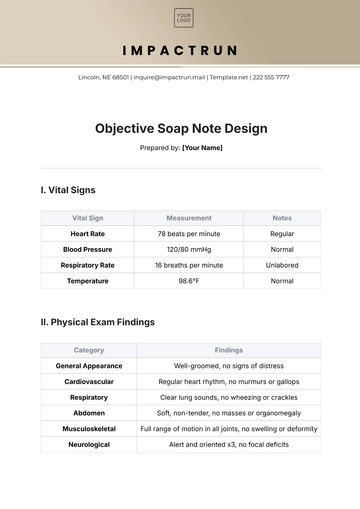
A. Vital Signs
Blood Pressure: 150/92 mmHg.
Heart Rate: 98 bpm.
Respiratory Rate: 20 breaths/min.
Temperature: 98.6°F.
B. Physical Examination
General Appearance: The patient appears anxious and mildly diaphoretic.
Cardiovascular: No murmurs, gallops, or rubs; S1 and S2 audible.
Respiratory: Clear lung sounds bilaterally, no crackles or wheezes.
Abdomen: Soft, non-tender, no organomegaly.
Extremities: No edema; peripheral pulses intact.
C. Diagnostic Tests
ECG: ST-segment depression noted in leads II, III, and aVF.
Troponin: Pending.
Chest X-ray: No abnormalities.
III. Assessment
Primary Diagnosis: Unstable angina.
Differential Diagnoses:
Acute coronary syndrome (ACS).
Gastroesophageal reflux disease (GERD).
Costochondritis.
IV. Plan
A. Immediate Interventions
Administered aspirin 325 mg and sublingual nitroglycerin.
Oxygen therapy was initiated at 2 L/min via nasal cannula.
B. Diagnostics
Repeat troponin levels in 6 hours.
Order echocardiogram.
Schedule a stress test if symptoms stabilize.
C. Medications
Prescribed beta-blocker (metoprolol 25 mg twice daily).
Statin therapy to manage hyperlipidemia (atorvastatin 40 mg daily).
D. Referrals
Refer to cardiology for further evaluation.
E. Follow-Up
Reassess in 24 hours or sooner if symptoms worsen.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Address critical care needs with Template.net's Chest Pain Soap Note Template. This fully editable and customizable tool is designed for swift, accurate documentation of chest pain cases. Utilize our Ai Editor Tool for precise, tailored notes, enhancing patient assessment and care in urgent medical situations.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note